Abstract
Objective
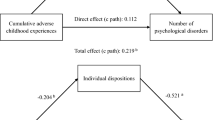
Research has demonstrated that adverse childhood experiences (ACEs) were related to elevated lifetime risk of developing obesity, but the underlying mechanisms between ACEs and development of obesity are yet to be fully elucidated. The current study aims to extend exiting evidence on underlying mechanisms between ACEs and development of obesity by examining whether depressive symptom and binge eating symptom have independently significant mediating effects on the association.
Methods
The study used data from a total of 473 patients seeking bariatric surgery who completed psychological evaluation including ACEs, depressive symptom, and binge eating scale as a part of presurgical multidisciplinary weight management consultations. Mediation analyses were conducted using the PROCESS macro for SPSS to examine the research objective.
Results
The study found that depressive symptom uniquely mediated the relationship between ACEs and obesity, but binge eating symptom did not significantly mediate the relationship independently of depression.
Conclusions
The unique role of depression in relation to childhood trauma in this study argues for more focus on a mental health intervention with bariatric patients during the preoperative period. Addressing ACEs for bariatric patients who present psychiatric symptoms during preoperative process could have potential benefits to patient care.
Graphical abstract



Similar content being viewed by others
References
Kadouh HC, Acosta A. Current paradigms in the etiology of obesity. Tech Gastrointest Endosc. 2017;19(1):2–11. https://doi.org/10.1016/j.tgie.2016.12.001.
Kim Y, Lee H, Park A. Adverse childhood experiences, economic hardship, and obesity: differences by gender. Child Youth Serv Rev. 2020; 116. https://doi.org/10.1016/j.childyouth.2020.105214.
Lodhia NA, Rosas US, Moore M, et al. Do adverse childhood experiences affect surgical weight loss outcomes? J Gastrointest Surg. 2015;19(6):993–8. https://doi.org/10.1007/s11605-015-2810-7.
Wiss DA, Brewerton TD. Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020;1(223):112964. https://doi.org/10.1016/j.physbeh.2020.112964.
Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–58.
Copeland WE, Keeler G, Angold A, et al. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry. 2007;64(5):577–84. https://doi.org/10.1001/archpsyc.64.5.577.
Finkelhor D, Ormrod RK, Turner HA. Lifetime assessment of poly-victimization in a national sample of children and youth. Child Abuse Negl. 2009;33(7):403–11. https://doi.org/10.1016/j.chiabu.2008.09.012.
Gardner R, Feely A, Layte R, et al. Adverse childhood experiences are associated with an increased risk of obesity in early adolescence: a population-based prospective cohort study. Pediatr Res. 2019;86(4):522–8. https://doi.org/10.1038/s41390-019-0414-8.
Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–66. https://doi.org/10.1016/S2468-2667(17)30118-4.
Elsenburg LK, van Wijk KJE, Liefbroer AC, et al. Accumulation of adverse childhood events and overweight in children: a systematic review and meta-analysis. Obesity (Silver Spring). 2017;25(5):820–32. https://doi.org/10.1002/oby.21797.
Fuemmeler BF, Dedert E, McClernon FJ, et al. Adverse childhood events are associated with obesity and disordered eating: results from a U.S. population-based survey of young adults. J Trauma Stress. 2009;22(4):329–33. https://doi.org/10.1002/jts.20421.
Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatry. 2014;19(5):544–54. https://doi.org/10.1038/mp.2013.54.
Shinagawa A, Ahrendt AJ, Epstein EM, et al. The association between adverse childhood experiences (ACEs) and postoperative bariatric surgery weight loss outcomes. Obes Surg. 2020;30(11):4258–66. https://doi.org/10.1007/s11695-020-04779-8.
Li M, D’Arcy C, Meng X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychol Med. 2016;46:717–30.
Park S, Hong JP, Bae JN, et al. Cho MJ Impact of childhood exposure to psychological trauma on the risk of psychiatric disorders and somatic discomfort single vs multiple types of psychological trauma. Psychiatry Res. 2014;219(3):443–9.
Vámosi M, Heitmann BL, Kyvik KO. The relation between an adverse psychological and social environment in childhood and the development of adult obesity: a systematic literature review. Obes Rev. 2010;11(3):177–84. https://doi.org/10.1111/j.1467-789X.2009.00645.x.
Dedert EA, Becker ME, Fuemmeler BF, et al. Childhood traumatic stress and obesity in women: the intervening effects of PTSD and MDD. J Trauma Stress. 2010;23(6):785–863. https://doi.org/10.1002/jts.20584.
Greenfield EA, Marks NF. Identifying experiences of physical and psychological violence in childhood that jeopardize mental health in adulthood. Child Abuse Negl. 2010;34(3):161–71. https://doi.org/10.1016/j.chiabu.2009.08.012.
Rohde P, Ichikawa L, Simon GE, et al. Associations of child sexual and physical abuse with obesity and depression in middle-aged women. Child Abuse Negl. 2008;32(9):878–87. https://doi.org/10.1016/j.chiabu.2007.11.004.
Shakory S, Van Exan J, Mills JS, et al. Binge eating in bariatric surgery candidates: the role of insecure attachment and emotion regulation. Appetite. 2015;91:69–75. https://doi.org/10.1016/j.appet.2015.03.026.
Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obes Relat Dis. 2016;12(4):731–49. https://doi.org/10.1016/j.soard.2016.02.008.
Dube SR, Williamson DF, Thompson T, et al. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004;28(7):729–37. https://doi.org/10.1016/j.chiabu.2003.08.009.
Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18(3):263–83. https://doi.org/10.1177/1073191111411667.
Gormally J, Black S, Daston S, et al. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. https://doi.org/10.1016/0306-4603(82)90024-7.
Freitas SR, Lopes CS, Appolinario JC, et al. The assessment of binge eating disorder in obese women: a comparison of the binge eating scale with the structured clinical interview for the DSM-IV. Eat Behav. 2006;7(3):282–9. https://doi.org/10.1016/j.eatbeh.2005.09.002.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. Guilford Press; 2017.
Pilkonis PA, Yu L, Dodds NE, et al. Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS) in a three-month observational study. J Psychiatr Res. 2014;56:112–9. https://doi.org/10.1016/j.jpsychires.2014.05.010.
Hood MM, Grupski AE, Hall BJ, et al. Factor structure and predictive utility of the Binge Eating Scale in bariatric surgery candidates. Surg Obes Relat Dis. 2013;9(6):942–8. https://doi.org/10.1016/j.soard.2012.06.013.
Wiss DA, Brewerton TD. Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020;223:112964. https://doi.org/10.1016/j.physbeh.2020.112964.
Michopoulos V, Powers A, Moore C, Villarreal S, Ressler KJ, Bradley B. The mediating role of emotion dysregulation and depression on the relationship between childhood trauma exposure and emotional eating. Appetite. 2015;91:129–36. https://doi.org/10.1016/j.appet.2015.03.036.
Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Attachment security and disorganization in maltreating and high-risk families: a series of meta-analyses. Dev Psychopathol. 2010;22(1):87–108. https://doi.org/10.1017/S0954579409990289.
Riggs SA. Childhood emotional abuse and the attachment system across the life cycle: what theory and research tell us. J Aggress Maltreat Trauma. 2010;19(1):5–51. https://doi.org/10.1080/10926770903475968.
Struck N, Krug A, Feldmann M, et al. Attachment and social support mediate the association between childhood maltreatment and depressive symptoms. J Affect Disord. 2020;273:310–7. https://doi.org/10.1016/j.jad.2020.04.041.
Taube-Schiff M, Van Exan J, Tanaka R, Wnuk S, Hawa R, Sockalingam S. Attachment style and emotional eating in bariatric surgery candidates: the mediating role of difficulties in emotion regulation. Eat Behav. 2015;18:36–40. https://doi.org/10.1016/j.eatbeh.2015.03.011.
Ty M, Francis AJ. Insecure attachment and disordered eating in women: the mediating processes of social comparison and emotion dysregulation. Eat Disord. 2013;21(2):154–74. https://doi.org/10.1080/10640266.2013.761089.
Rasmusson G, Lydecker JA, Coffino JA, White MA, Grilo CM. Household food insecurity is associated with binge-eating disorder and obesity [published online ahead of print, 2018 Dec 19]. Int J Eat Disord. 2018. https://doi.org/10.1002/eat.22990.
Grilo CM, Masheb RM. Childhood psychological, physical, and sexual maltreatment in outpatients with binge eating disorder: frequency and associations with gender, obesity, and eating-related psychopathology. Obes Res. 2001;9(5):320–5. https://doi.org/10.1038/oby.2001.40.
Park A, Kim Y. Adverse childhood experiences, economic hardship, and obesity: differences by gender, Child Youth Serv Rev. 2018;34–40. https://doi.org/10.1016/j.childyouth.2018.02.012
Clark MM, Hanna BK, Mai JL, et al. Sexual abuse survivors and psychiatric hospitalization after bariatric surgery. Obes Surg. 2007;17(4):465–9. https://doi.org/10.1007/s11695-007-9084-4.
Fink K, Ross CA. Adverse childhood experiences in a post-bariatric surgery psychiatric inpatient sample. Obes Surg. 2017;27(12):3253–7. https://doi.org/10.1007/s11695-017-2767-6.
Kinzl JF, Schrattenecker M, Traweger C, et al. Psychosocial predictors of weight loss after bariatric surgery. Obes Surg. 2006;16(12):1609–14. https://doi.org/10.1381/096089206779319301.
Holzer SR, Uppala S, Wonderlich SA, et al. Mediational significance of PTSD in the relationship of sexual trauma and eating disorders. Child Abuse Negl. 2008;32(5):561–6. https://doi.org/10.1016/j.chiabu.2007.07.011.
Karmali S, Brar B, Shi X, et al. Weight recidivism post-bariatric surgery: a systematic review. Obes Surg. 2013;23(11):1922–33. https://doi.org/10.1007/s11695-013-1070-4
Leung SE, Wnuk S, Jackson T, et al. Sockalingam S Prospective study of attachment as a predictor of binge eating, emotional eating and weight loss two years after bariatric surgery. Nutrients. 2019;11(7):1625. https://doi.org/10.3390/nu11071625.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
This does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
The relationship between ACEs and adult obesity has been well documented, but little is known on the underlying mechanisms between them.
Depression uniquely mediated the relationship between ACEs and obesity, but not binge eating.
Providing additional intervention to bariatric patients who were identified to have psychiatric symptoms related to childhood trauma may help to achieve better health improvement.
Rights and permissions
About this article
Cite this article
Tabone, J.K., Cox, S., Aylward, L. et al. The Roles of Depression and Binge Eating in the Relationship Between Adverse Childhood Experiences (ACEs) and Obesity. OBES SURG 32, 3034–3040 (2022). https://doi.org/10.1007/s11695-022-06192-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06192-9