Abstract
Purpose
The use of intragastric balloons (IGBs) for the treatment of obesity was approved by the US Food and Drug Administration in 2015. This study aims to characterize preoperative factors and outcomes of patients undergoing IGB therapy compared to bariatric surgery (non-IGB) and evaluate 5-year trends in IGB use.
Methods
A retrospective cohort study was performed by extracting data from the MBSAQIP registry between 2015 and 2019. All non-IGB and IGB procedures were included while revisional and emergency surgeries were excluded. Multivariable logistic regression analysis was used to determine independent predictors of patient selection for IGB therapy.
Results
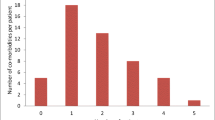
Of 652,927 patients identified, only 2910 (0.4%) underwent IGB therapy. Patients who underwent IGB therapy were older (46.7 ± 11.4 years vs 44.4 ± 12.0 years; p < 0.0001), had lower BMI at baseline (37.0 ± 6.2 kg/m2 vs 45.3 ± 7.8 kg/m2; p < 0.0001), and were overall healthier with fewer comorbidities and better functional status. The rate of early nonoperative reintervention was higher in the IGB cohort (7.7% vs 1.1%; p < 0.0001). Age was the only significant predictor of selection for IGB therapy (OR 1.32; 95% CI 1.24–1.37; p < 0.0001). The number of IGB procedures reported between 2016 and 2019 declined significantly (953 (0.62%) vs 418 (0.25%); p < 0.0001).
Conclusions
Appropriate indications for IGBs appear to be increasingly limited. The ongoing role of IGBs in the treatment of obesity is unclear given the safety and efficacy of modern bariatric surgery and new pharmacological agents for weight loss.
Graphical abstract

Similar content being viewed by others
References
Gasoyan H, et al. Reasons for underutilization of bariatric surgery: the role of insurance benefit design. Surg Obes Relat Dis. 2019;15(1):146–51.
Nieben OG, Harboe H. Intragastric balloon as an artificial bezoar for treatment of obesity. Lancet. 1982;1(8265):198–9.
Gleysteen JJ. A history of intragastric balloons. Surg Obes Relat Dis. 2016;12(2):430–5.
Moura D, et al. Effectiveness of intragastric balloon for obesity: a systematic review and meta-analysis based on randomized control trials. Surg Obes Relat Dis. 2016;12(2):420–9.
Saber AA, et al. Efficacy of first-time intragastric balloon in weight loss: a systematic review and meta-analysis of randomized controlled trials. Obes Surg. 2017;27(2):277–87.
Schapiro M, et al. Obesity and the gastric balloon: a comprehensive workshop. Tarpon Springs, Florida, March 19–21, 1987. Gastrointest Endosc, 1987. 33(4): p. 323–7.
Ponce J, et al. The REDUCE pivotal trial: a prospective, randomized controlled pivotal trial of a dual intragastric balloon for the treatment of obesity. Surg Obes Relat Dis. 2015;11(4):874–81.
Courcoulas A, et al. Intragastric balloon as an adjunct to lifestyle intervention: a randomized controlled trial. Int J Obes (Lond). 2017;41(3):427–33.
Ali MR, et al. American Society for Metabolic and Bariatric Surgery position statement on intragastric balloon therapy endorsed by the Society of American Gastrointestinal and Endoscopic Surgeons. Surg Obes Relat Dis. 2016;12(3):462–7.
Livingston EH, et al. National Surgical Quality Improvement Program analysis of bariatric operations: modifiable risk factors contribute to bariatric surgical adverse outcomes. J Am Coll Surg. 2006;203(5):625–33.
Verhoeff K. et al. Five years of MBSAQIP data: characteristics, outcomes, and trends for patients with super-obesity. Obes Surg, 2021.
Mocanu V, et al. Preoperative weight loss is linked to improved mortality and leaks following elective bariatric surgery: an analysis of 548,597 patients from 2015–2018. Surg Obes Relat Dis. 2021;17(11):1846–53.
Busetto L, et al. Preoperative weight loss by intragastric balloon in super-obese patients treated with laparoscopic gastric banding: a case-control study. Obes Surg. 2004;14(5):671–6.
Administration, U.S.F.a.D. Summary of safety and effectiveness data (SSED). ReShape™ Integrated Dual Balloon System – P140012. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf14/p140012b.pdf. Accessed 18 Dec 2021
Administration, U.S.F.a.D. Summary of safety and effectiveness data (SSED). ORBERA™ Intragastric Balloon System - P140008. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf14/P140008c.pdf. Accessed 18 December 2021
Eid GM, et al. Laparoscopic sleeve gastrectomy for super obese patients: forty-eight percent excess weight loss after 6 to 8 years with 93% follow-up. Ann Surg. 2012;256(2):262–5.
Milone L, Strong V, Gagner M. Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI > or =50). Obes Surg. 2005;15(5):612–7.
Dang JT, et al. Evaluating the safety of intragastric balloon: an analysis of the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. Surg Obes Relat Dis. 2018;14(9):1340–7.
Neto MG, et al. Brazilian Intragastric Balloon Consensus Statement (BIBC): practical guidelines based on experience of over 40,000 cases. Surg Obes Relat Dis. 2018;14(2):151–9.
Yorke E, et al. Intragastric balloon for management of severe obesity: a systematic review. Obes Surg. 2016;26(9):2248–54.
Kotzampassi K, et al. 500 intragastric balloons: what happens 5 years thereafter? Obes Surg. 2012;22(6):896–903.
Yanovski SZ, Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA. 2014;311(1):74–86.
Wilding JPH, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent does not apply for this type of study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• The use of IGBs at MBSAQIP centers has declined over the past 5 years
• IGBs are primarily used in older healthier patients with lower BMI
• Rates of early reintervention are higher with IGBs than with bariatric surgery
• The ongoing role of IGBs in the treatment of obesity is unclear
Rights and permissions
About this article
Cite this article
Chow, A., Mocanu, V., Verhoeff, K. et al. Trends in the Utilization of Intragastric Balloons: a 5-Year Analysis of the MBSAQIP Registry. OBES SURG 32, 1649–1657 (2022). https://doi.org/10.1007/s11695-022-06005-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06005-z