Abstract
Purpose
Metabolic dysfunction–associated fatty liver disease–related cirrhosis is possible at the time of bariatric surgery, complicated by further liver decompensation. Hepatic decompensation can also occur in the absence of cirrhosis but the presentation is less clear.
Methods
We analyze the clinical characteristics, histological findings, and management of patients without cirrhosis who developed hepatic decompensation after bariatric surgery in our single tertiary-care hospital.
Results
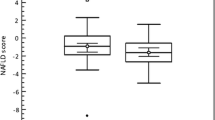
From 2014 to 2019, 6 patients underwent a transvenous liver biopsy for liver decompensation after bariatric surgery. Mean age at diagnosis was 44 years. The time between bariatric surgery and the onset of symptoms varied widely (min. 8 months, max. 17 years). Mean % of weight loss was high at 43%. The clinical presentation was as follows: fatigue and jaundice (5/6), leg edema (3/6), and ascites (1/6). Blood test showed increased transaminases (mean ALT 53 UI/L, mean AST 130 UI/L), bilirubin (mean 6 mg/dL), and INR (mean 1.5) with a low albumin level (mean 27 mg/dL). The hepatic venous pressure gradient was high (mean 10 mmHg). Histology revealed steatosis, hepatocyte ballooning but also portal inflammation with polymorphonuclear cells, and bile duct alterations. Mean fibrosis score was 2. The clinical course was favorable with nutritional support with a mean follow-up of 36 months.
Conclusion
Liver decompensation in the absence of cirrhosis can occur after bariatric surgery with a highly variable delay. A special histological signature is present with the coexistence of steatosis, bile duct alterations, and portal inflammation. Substantial clinical improvement with appropriate nutritional support seems to be effective.
Graphical abstract




Similar content being viewed by others
References
Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018:437–43.
Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:1495–7.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. J Am Med Assoc. 2004:1724–37.
Lassailly G, Caïazzo R, Pattou F, et al. Bariatric surgery for curing NASH in the morbidly obese? J Hepatol. 2013:1249–51.
La LN. NASH en 2018. Louv Med. 2018;137:308–13.
Lanthier N. Physiopathologie de la NASH: de nouveaux facteurs de risque identifiés ? Louv Med. 2020;139:405–10.
Lanthier N, Vanuytsel T. Metabolic dysfunction-associated fatty liver disease: a new clearer nomenclature with positive diagnostic criteria. Acta Gastroenterol Belg. 2020:513–5.
Ahmed S, Pouwels S, Parmar C, et al. Outcomes of bariatric surgery in patients with liver cirrhosis: a systematic review. Obes. Surg. 2021:1518–26.
Lanthier N. New therapies in non-alcoholic steatohepatitis | Les nouveaux traitements de la stéatohépatite non-alcoolique. Nutr Clin Metab. 2020;34:216–22.
King WC, Chen JY, Courcoulas AP, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017;13:1392–402.
Lefere S, Stroobant L, Verhelst X, et al. Bariatric surgery patients are at risk for alcoholic liver disease with need for liver transplantation. Obes Surg. 2020;30:4659–64.
Mendoza YP, Becchetti C, Wan T, et al. Malnutrition and alcohol in patients presenting with severe complications of cirrhosis after laparoscopic bariatric surgery. Obes Surg. 2021;31:2817–22.
Mahawar KK, Parmar C, Graham Y, et al. Monitoring of liver function tests after Roux-en-Y gastric bypass: an examination of evidence base. Obes Surg. 2016:2516–22.
D’Albuquerque LAC, Gonzalez AM, Wahle RC, et al. Liver transplantation for subacute hepatocellular failure due to massive steatohepatitis after bariatric surgery. Liver Transplant. 2008;14:881–5.
Lefere S, Hoorens A, Raevens S, et al. Refractory subacute steatohepatitis after biliopancreatic diversion. Hepatology. 2017;66:289–91.
Geerts A, Darius T, Chapelle T, et al. The multicenter Belgian survey on liver transplantation for hepatocellular failure after bariatric surgery. Transplant Proc. 2010:4395–8.
Lanthier N, Rubbia-Brandt L, Lin-Marq N, et al. Hepatic cell proliferation plays a pivotal role in the prognosis of alcoholic hepatitis. J Hepatol. 2015;63:609–21.
Lanthier N, Lin-Marq N, Rubbia-Brandt L, et al. Autologous bone marrow-derived cell transplantation in decompensated alcoholic liver disease: what is the impact on liver histology and gene expression patterns? Stem Cell Res Ther. 2017;8.
Bedossa P, Poitou C, Veyrie N, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–9.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Bischoff SC, Bernal W, Dasarathy S, et al. ESPEN practical guideline: clinical nutrition in liver disease. Clin Nutr. 2020;39:3533–62.
Sax HC. Long-term morbidity following jejunoileal bypass: the continuing potential need for surgical reversal. J Parenter Enter Nutr. 1995;19:328–9.
Lowell JA, Shenoy S, Ghalib R, et al. Liver transplantation after jejunoileal bypass for morbid obesity. J Am Coll Surg. 1997;185:123–7.
Silver HJ, Torquati A, Jensen GL. Weight, dietary and physical activity behaviors two years after gastric bypass. Obes Surg. 2006;16:859–64.
Ignat M, Vix M, Imad I, et al. Randomized trial of Roux-en-Y gastric bypass versus sleeve gastrectomy in achieving excess weight loss. Br J Surg. 2017;104:248–56.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity. 2013;21:1519–25.
Celebi G, Cicek AF, Gurel H, et al. Microvesicular steatosis: a missed item in the management of nonalcoholic fatty liver disease? Acta Gastroenterol Belg. 2020;83:565–70.
Tandra S, Yeh MM, Brunt EM, et al. Presence and significance of microvesicular steatosis in nonalcoholic fatty liver disease. J Hepatol. 2011;55:654–9.
Brunt EM, Janney CG, Di Bisceglie AM. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–74.
van Dongen JL, Michielsen PP, Van den Eynden GG, et al. Rapidly evolving liver decompensation with some remarkable features 14 years after biliopancreatic derivation: a case report and literature review. Acta Gastroenterol Belg. 2010:46–51.
Addeo P, Cesaretti M, Anty R, et al. Liver transplantation for bariatric surgery-related liver failure: a systematic review of a rare condition. Surg Obes Relat Dis. 2019;15:1394–401.
Lal S, Pironi L, Wanten G, et al. Clinical approach to the management of intestinal failure associated liver disease (IFALD) in adults: a position paper from the Home Artificial Nutrition and Chronic Intestinal Failure Special Interest Group of ESPEN. Clin Nutr. 2018;37:1794–7.
Buchman AL, Naini BV, Spilker B. The differentiation of intestinal-failure-associated liver disease from nonalcoholic fatty liver and nonalcoholic steatohepatitis. Semin Liver Dis. 2017:33–44.
Lanthier N, Stärkel P, Dahlqvist G. Muscle mass depletion in chronic liver diseases: an accelerated model of aging or a distinct entity? Clin Res Hepatol Gastroenterol. 2021;45:101721.
Lammers WJ, van Tilburg AJP, Apers JA, et al. Liver failure caused by prolonged state of malnutrition following bariatric surgery. World J Hepatol. 2018;10:396–9.
Mocanu I, Carvalhana S, Costa P, et al. Liver-failure-after-bariatric-surgery-clinical-case-and-literature-review. J Gastroenterol Metab. 2018;1:1–4.
Gonçalves DC, Lira FS, Yamashita AS, et al. Liver lipid metabolism disruption in cancer cachexia is aggravated by CLA supplementation -induced inflammation. Clin Nutr. 2019;38:2219–30.
Ralki M, Cassiman D, Van Dongen J, et al. Liver failure after long-limb gastric bypass. Clin Res Hepatol Gastroenterol. 2017;41:e32–7.
Takeuchi M, Vidigal PT, Guerra MT, et al. Neutrophils interact with cholangiocytes to cause cholestatic changes in alcoholic hepatitis. Gut. 2021;70:342–56.
Lanthier N, Stärkel P. Treatment of severe alcoholic hepatitis: past, present and future. Eur J Clin Invest. 2017:531–9.
Zaccherini G, Bernardi M. The role and indications of albumin in advanced liver disease. Acta Gastroenterol Belg. 2019:301–8.
Acknowledgements
Nicolas Lanthier is a post-doctoral researcher from the Fonds de la Recherche Scientifique (FNRS), Belgium.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the ethical committee (Commission d’éthique hospitalo-facultaire, Cliniques universitaires Saint-Luc, UCLouvain) with the following reference: 2021/16MAR/129. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of retrospective study, formal consent was not required.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Liver damage and decompensation can occur after bariatric surgery, even in the absence of cirrhosis.
• A special histological signature is present with the coexistence of steatosis, bile duct alterations, and portal inflammation.
• Severe weight loss, protein malnutrition, and bacterial overgrowth are a possible cause.
• The treatment is appropriate nutritional support.
Rights and permissions
About this article
Cite this article
Vande Berg, P., Ulaj, A., de Broqueville, G. et al. Liver Decompensation after Bariatric Surgery in the Absence of Cirrhosis. OBES SURG 32, 1227–1235 (2022). https://doi.org/10.1007/s11695-022-05930-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-05930-3