Abstract
Purpose
Clinically severe obesity (SO) is a known risk factor for worsened outcomes and recurrence of acute diverticulitis. Paucity of data exist on outcomes of diverticulitis after bariatric surgery.
Methods
The Nationwide Readmissions Database was queried for diverticulitis hospitalizations between the years 2010 and 2014. We restricted analysis to patients with SO and those who had bariatric surgery (BRS). Outcomes of mortality, surgical events, and recurrent diverticulitis admissions were compared using multivariable analysis and one-to-one propensity score matching.
Results
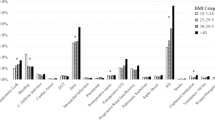
Among 52,274 diverticulitis admissions, 91.2% (47,694) patients had SO and 8.8% (4580) had prior BRS. Patients with SO had higher odds of suffering mortality on index diverticulitis admission when compared to those with prior BRS [adjusted odds ratio (aOR): 10.55; 95%CI 1.45,76.75]. Patients with SO were also more likely to undergo emergency surgery (aOR: 1.71; 95%CI 1.25,2.34) and colectomy (aOR: 1.45; 95%CI 1.26,1.68). Rates of recurrent diverticulitis readmissions within 30 days and 6 months were also higher in patients with SO compared to BRS patients (aOR: 7.94; 95%CI 1.09,57.83 and aOR: 1.98; 95%CI 1.14,3.43, respectively). Propensity score matching confirmed our findings of increased rates of mortality (OR: 17.28; 95%CI 2.02,147.6), recurrent diverticulitis, and worsened surgical outcomes within 30 days in patients with SO compared to BRS.
Conclusion
This study is first to show improved outcomes and less recurrent hospitalizations for diverticulitis after bariatric surgery compared to patients with clinically severe obesity. Further studies are needed to understand mechanisms leading to this improvement and the role of weight loss in prevention of severe diverticulitis.
Graphical abstract


Similar content being viewed by others
Abbreviations
- AOR:
-
Adjusted odds ratios
- AHRQ:
-
Agency for Healthcare Research and Quality
- BMI:
-
Body mass index
- CI:
-
Confidence intervals
- HCUP:
-
Healthcare Cost Utilization Project
- ICU:
-
Intensive care unit
- ICD-9-CM:
-
International Classification of Diseases, Ninth Revision, Clinical Modification
- IQR:
-
Interquartile range
- NRD:
-
Nationwide Readmission Database
- OR:
-
Odds ratios
- SE:
-
Standard error
- SID:
-
State inpatient databases
- SO:
-
Clinically severe obesity
- US:
-
United States
References
Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterol. 2009;136(3):741–54.
Peery AF, Crockett SD, Murphy CC, et al. Burden and Cost of Gastrointestinal Liver and Pancreatic Diseases in the United States: Update 2018. Gastroenterol. 2019;156(1):254-272.e211.
Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal Trends in the Incidence and Natural History of Diverticulitis A Population-Based Study. Am J Gastroenterol. 2015;110(11):1589–96.
Etzioni DA, Mack TM, Beart RW, Kaiser AM. Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg. 2009;249(2):210–7.
Strate LL, Morris AM. Epidemiology Pathophysiology and Treatment of Diverticulitis. Gastroenterology. 2019;156(5):1282-1298.e1281.
Reja D, Weisberg I. Risk factors and incidence of 90-day readmission for diverticulitis after an acute diverticulitis index admission. Int J Colorectal Dis. 2021;36(2):347–52.
Afshin A, Forouzanfar MH, Reitsma MB, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377(1):13–27.
(NCD-RisC) NRFC. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet. 2016;387(10026):1377–96.
Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in Obesity Among Adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–91.
Docimo S, Lee Y, Chatani P, Rogers AM, Lacqua F. Visceral to subcutaneous fat ratio predicts acuity of diverticulitis. Surg Endosc. 2017;31(7):2808–12.
Patel K, Krishna SG, Porter K, et al. Diverticulitis in Morbidly Obese Adults: A Rise in Hospitalizations with Worse Outcomes According to National US Data. Dig Dis Sci. 2020;65(9):2644–53.
El-Sayed C, Radley S, Mytton J, Evison F, Ward ST. Risk of Recurrent Disease and Surgery Following an Admission for Acute Diverticulitis. Dis Colon Rectum. 2018;61(3):382–9.
O’Brien PE, Hindle A, Brennan L, et al. Long-Term Outcomes After Bariatric Surgery: a Systematic Review and Meta-analysis of Weight Loss ator More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obes Surg. 2019;29(1):3–14.
Park CH, Nam SJ, Choi HS, et al. Comparative Efficacy of Bariatric Surgery in the Treatment of Morbid Obesity and Diabetes Mellitus: a Systematic Review and Network Meta-Analysis. Obes Surg. 2019;29(7):2180–90.
Healthcare Cost and Utilization Project (HCUP). 2007 2008, 2009, 2010, 2011, 2007.
NRD Overview. Healthcare Cost and Utilization Project (HCUP) December 2019; Overview of the Nationwide Readmissions Database (NRD). Available at: https://www.hcup-us.ahrq.gov/nrdoverview.jsp.
Kruger AJ, Mumtaz K, Anaizi A, et al. Cirrhosis Is Associated with Increased Mortality in Patients with Diverticulitis: A Nationwide Cross-Sectional Study. Dig Dis Sci. 2017;62(11):3149–55.
Kassam Z, Cribb Fabersunne C, Smith MB, et al. Clostridium difficile associated risk of death score (CARDS): a novel severity score to predict mortality among hospitalised patients with C. difficile infection. Alimentary pharmacology & therapeutics. 2016;43(6):725–33.
Hussan H, Gray DM, 2nd, Hinton A, Krishna SG, Conwell DL, Stanich PP. Morbid Obesity is Associated with Increased Mortality, Surgical Complications, and Incremental Health Care Utilization in the Peri-Operative Period of Colorectal Cancer Surgery. World journal of surgery. Dec 7 2015.
Masoomi H, Buchberg BS, Magno C, Mills SD, Stamos MJ. Trends in diverticulitis management in the united states from 2002 to 2007. Arch Surg. 2011;146(4):400–6.
Schlussel AT, Lustik MB, Cherng NB, Maykel JA, Hatch QM, Steele SR. Right-sided diverticulitis requiring colectomy: an evolving demographic? a review of surgical outcomes from the National Inpatient Sample Database. J Gastrointest Surg. 2016;20(11):1874–85.
Lenis D, Nguyen TQ, Dong N, Stuart EA. It’s all about balance: propensity score matching in the context of complex survey data. Biostatistics. 2019;20(1):147–63.
Austin PC, Jembere N, Chiu M. Propensity score matching and complex surveys. Stat Methods Med Res. 2018;27(4):1240–57.
Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB. Variation in Outcomes at Bariatr. JAMA Surg. 2017;152(7):629–36.
Ho VP, Nash GM, Milsom JW, Lee SW. Identification of diverticulitis patients at high risk for recurrence and poor outcomes. J Trauma Acute Care Surg. 2015;78(1):112–9.
van de Wall BJ, Poerink JA, Draaisma WA, Reitsma JB, Consten EC, Broeders IA. Diverticulitis in young versus elderly patients: a meta-analysis. Scand J Gastroenterol. 2013;48(6):643–51.
Cox AJ, West NP, Cripps AW. Obesity, inflammation, and the gut microbiota. Lancet Diabetes Endocrinol. 2015;3(3):207–15.
Cancello R, Henegar C, Viguerie N, et al. Reduction of macrophage infiltration and chemoattractant gene expression changes in white adipose tissue of morbidly obese subjects after surgery-induced weight loss. Diabetes. 2005;54(8):2277–86.
Habib P, Scrocco JD, Terek M, Vanek V, Mikolich JR. Effects of bariatric surgery on inflammatory, functional and structural markers of coronary atherosclerosis. Am J Cardiol. 2009;104(9):1251–5.
Moschen AR, Molnar C, Geiger S, et al. Anti-inflammatory effects of excessive weight loss: potent suppression of adipose interleukin 6 and tumour necrosis factor alpha expression. Gut. 2010;59(9):1259–64.
Magouliotis DE, Tasiopoulou VS, Sioka E, Chatedaki C. Zacharoulis D Impact of Bariatric Surgery on Metabolic and Gut Microbiota Profile: a Systematic Review and Meta-analysis. Obesity Surg. 2017;27(5):1345–57.
Panteliou E, Miras AD. What is the role of bariatric surgery in the management of obesity? Climacteric. 2017;20(2):97–102.
Mathews SN, Lamm R, Yang J, et al. Factors Associated with Repeated Health Resource Utilization in Patients with Diverticulitis. J Gastrointest Surg. 2017;21(1):112–20.
Mehta D, Saha A, Chawla L, et al. National Landscape of Unplanned 30-Day Readmission Rates for Acute Non-hemorrhagic Diverticulitis: Insight from National Readmission Database. Dig Dis Sci. 2020.
Al-Masrouri S, Garfinkle R, Al-Rashid F, et al. Readmission for Treatment Failure After Nonoperative Management of Acute Diverticulitis: A Nationwide Readmissions Database Analysis. Dis Colon Rectum. 2020;63(2):217–25.
Jamal Talabani A, Endreseth BH, Lydersen S, Edna TH. Clinical diagnostic accuracy of acute colonic diverticulitis in patients admitted with acute abdominal pain, a receiver operating characteristic curve analysis. Int J Colorectal Dis. 2017;32(1):41–7.
McLynn RP, Geddes BJ, Cui JJ, et al. Inaccuracies in ICD Coding for Obesity Would Be Expected to Bias Administrative Database Spine Studies Toward Overestimating the Impact of Obesity on Perioperative Adverse Outcomes. Spine (Phila Pa 1976). 2018;43(7):526–32.
Funding
We did not rely on grant support or other assistance for this manuscript.
Author information
Authors and Affiliations
Contributions
Dr. Patel was involved in the design, data interpretation, and drafting and critical revision of the manuscript. Mr. Porter was involved in the study’s design, acquiring and statistically analyzing the data, and critical revision of the manuscript. Drs. Krishna, Needleman, Brethauer, and Conwell were involved in the design, data interpretation, and critical revision of the manuscript. Dr. Hussan was involved in the conception, design, interpretation of data, and the manuscript’s drafting and critical revision.
Corresponding author
Ethics declarations
Ethics Statement
For this type of study formal consent is not required given that data contained within the NRD are neither identifiable nor private and thus do not meet the federal definition of ‘‘human subject’.’
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
- Patients with prior bariatric surgery had improved outcomes in diverticulitis.
- These patients had less mortality, lower rates of surgery with less complications.
- These patients also had lower rates of recurrent diverticulitis admissions.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Patel, K., Porter, K., Krishna, S.G. et al. The Impact of Bariatric Surgery on Diverticulitis Outcomes and Risk of Recurrent Hospitalizations in Adults with Clinically Severe Obesity. OBES SURG 32, 365–373 (2022). https://doi.org/10.1007/s11695-021-05764-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05764-5