Abstract
Purpose
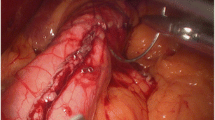
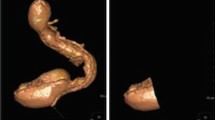
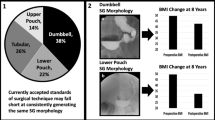
Laparoscopic sleeve gastrectomy (SG) is now frequently performed as a definitive bariatric procedure. The aim of the study was to evaluate the detailed morphology of remnant stomachs after SG with respect to volume and sleeve migration.
Materials and Methods
We performed a review of prospectively collected data on patients that completed a 12-month postop examination, which included CT volumetry of the sleeve, and a questionnaire that addressed postop food tolerance. CT volumetry study included total sleeve volume (TSV), tube volume (TV), antral volume (AV), tube/antral volume ratio (TAVR), and the presence of intrathoracic sleeve migration (ITSM).
Results
One hundred patients were included in this study. Mean %TWL (total weight loss) at 12 months postop was 31.1% (14.3~55.5), and mean TSV, TV, AV, and TAVR were 188.3 ± 67.3 ml, 81.3 ± 38.5 ml. 107.0 ± 45.1 ml, and 0.846 ± 0.514 respectively. TSV was not correlated significantly with %TWL at 12 months postop (r=−0.140, p=0.164). Thirty patients (30/100, 30%) showed ITSM. Patients with ITSM had a significantly lower mean GER score (5.9 ± 2.3 vs. 7.5±1.9, p=0.001), and a higher proportion showed suboptimal weight loss (43.3% vs. 15.7%, p=0.003).
Conclusions
Mean TSV was not found to be significantly correlated with %TWL at 12 months postop. The presence of ITSM indicated more frequent GER symptoms and a higher probability of suboptimal weight loss.
Graphical abstract







Similar content being viewed by others
References
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes Surg. 2017;27:2279–89.
Angrisani L, Santonicola A, Iovino P, et al. IFSO Worldwide Survey 2016: Primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy-a systematic review. Obes Surg. 2016;26:1326–34.
Saba J, Bravo M, Rivas E, et al. Incidence of de novo hiatal hernia after laparoscopic sleeve gastrectomy. Obes Surg. 2020;30:3730–4.
Coupaye M, Gorbatchef C, Calabrese D, et al. Gastroesophageal reflux after sleeve gastrectomy: a prospective mechanistic study. Obes Surg. 2018;28:838–45.
Suter M, Calmes JM, Paroz A, et al. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17:2–8.
Lazoura O, Zacharoulis D, Triantafyllidis G, et al. Symptoms of gastroesophageal reflux following laparoscopic sleeve gastrectomy are related to the final shape of the sleeve as depicted by radiology. Obes Surg. 2011;21:295–9.
Poublon N, Chidi I, Bethlehem M, et al. One anastomosis gastric bypass vs. Roux-en-Y gastric bypass, remedy for insufficient weight loss and weight regain after failed restrictive bariatric surgery. Obes Surg. 2020;30:3287–94.
Hanssen A, Plotnikov S, Acosta G, et al. 3D Volumetry and its correlation between postoperative gastric volume and excess weight loss after sleeve gastrectomy. Obes Surg. 2018;28:775–80.
Elbanna H, Emile S, El-Hawary GE, et al. Assessment of the correlation between preoperative and immediate postoperative gastric volume and weight loss after sleeve gastrectomy using computed tomography volumetry. World J Surg. 2019;43:199–206.
Pawanindra L, Vindal A, Midha M, et al. Early post-operative weight loss after laparoscopic sleeve gastrectomy correlates with the volume of the excised stomach and not with that of the sleeve! Preliminary data from a multi-detector computed tomography-based study. Surg Endosc. 2015;29:2921–7.
Disse E, Pasquer A, Pelascini E, et al. Dilatation of sleeve gastrectomy: myth or reality? Obes Surg. 2017;27:30–7.
Bakr AA, Fahmy MH, Elward AS, et al. Analysis of medium-term weight regain 5 years after laparoscopic sleeve gastrectomy. Obes Surg. 2019;29:3508–13.
Alvarez V, Carrasco F, Cuevas A, et al. Mechanisms of long-term weight regain in patients undergoing sleeve gastrectomy. Nutrition. 2016;32:303–8.
Fahmy MH, Sarhan MD, Osman AM, et al. Early weight recidivism following laparoscopic sleeve gastrectomy: a prospective observational study. Obes Surg. 2016;26:2654–60.
Lakdawala MA, Bhasker A, Mulchandani D, et al. Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study. Obes Surg. 2010;20:1–6.
Braghetto I, Csendes A, Korn O, et al. Gastroesophageal reflux disease after sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:148–53.
Himpens J, Dapri G, Cadiere GB. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16:1450–6.
Al-Sanea O, Al-Garzaie A, Dernaika M, et al. Rare complication post sleeve gastrectomy: Acute irreducible paraesophageal hernia. Int J Surg Case Rep. 2015;8C:88–91.
Saber AA, Shoar S, Khoursheed M. Intra-thoracic sleeve migration (ITSM): an underreported phenomenon after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27:1917–23.
Amor IB, Debs T, Kassir R, et al. De novo hiatal hernia of the gastric tube after sleeve gastrectomy. Int J Surg Case Rep. 2015;15:78–80.
Runkel N. The Gastric Migration Crisis in Obesity Surgery. Obes Surg. 2019;29:2301–2.
Hyun JJ, Bak YT. Clinical significance of hiatal hernia. Gut Liver. 2011;5:267–77.
Arnoldner MA, Felsenreich DM, Langer FB, et al. Pouch volume and pouch migration after Roux-en-Y gastric bypass: a comparison of gastroscopy and 3 D-CT volumetry: is there a “migration crisis”? Surg Obes Relat Dis. 2020;16:1902–8.
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicenter study. Obes Surg. 2019;29:1462–9.
Angrisani L, Santonicola A, Hasani A, et al. Five-year results of laparoscopic sleeve gastrectomy: effects on gastroesophageal reflux disease symptoms and co-morbidities. Surg Obes Relat Dis. 2016;12:960–8.
McGrice M, Don PK. Interventions to improve long-term weight loss in patients following bariatric surgery: challenges and solutions. Diabetes Metab Syndr Obes. 2015;8:263–74.
Van Wieren IA, Thumma JR, Obeid NR, et al. The influence of gastroesophageal reflux symptoms on patient satisfaction after sleeve gastrectomy. Surgery. 2019;166:873–8.
Vage V, Behme J, Jossart G, et al. Gastropexy predicts lower use of acid-reducing medication after laparoscopic sleeve gastrectomy. A prospective cohort study. Int J Surg. 2020;74:113–7.
Soong TC, Almalki OM, Lee WJ, et al. Revision of sleeve gastrectomy with hiatal repair with gastropexy for gastroesophageal reflux disease. Obes Surg. 2019;29:2381–6.
Lye TJY, Ng KR, Tan AWE, et al. Small hiatal hernia and postprandial reflux after vertical sleeve gastrectomy: a multiethnic Asian cohort. PLoS One. 2020;15:e0241847.
Lewis KH, Callaway K, Argetsinger S, et al. Concurrent hiatal hernia repair and bariatric surgery: outcomes after sleeve gastrectomy and Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2021;17:72–80.
Che F, Nguyen B, Cohen A, et al. Prevalence of hiatal hernia in the morbidly obese. Surg Obes Relat Dis. 2013;9:920–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Choi, S.J., Kim, S.M. Intrathoracic Migration of Gastric Sleeve Affects Weight Loss as well as GERD–an Analysis of Remnant Gastric Morphology for 100 Patients at One Year After Laparoscopic Sleeve Gastrectomy. OBES SURG 31, 2878–2886 (2021). https://doi.org/10.1007/s11695-021-05354-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05354-5