Abstract
Purpose
The reported incidence of surgical site infection (SSI) following bariatric surgery ranges from 1.4 to 30%. The use of skin staples and tissue adhesive was shown to be superior to sutures in reducing SSI in a variety of surgical disciplines; however, this area is under-investigated in elective bariatric surgery. The aim of this study was to examine the effect of tissue adhesive for skin closure on SSI in patients undergoing bariatric surgery.
Methods
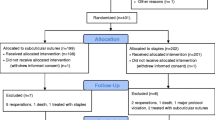
A retrospective analysis was performed to determine the incidence of SSI in patients who underwent elective laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG). Tissue adhesive was selectively used for skin closure during the study period. Patient characteristics, operative data, and 30-day postoperative outcomes were collected from patient charts and the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database.
Results
A total of 1,579 patients were included in the study. Tissue adhesive was used in 31.2% of all operations (n = 494). The rate of incisional SSI in our study was 2.2% (n = 35). The use of tissue adhesive was more common in patients who developed incisional SSI compared with those without incisional SSI (54.3 vs. 30.8%, p = 0.003). On multivariate analysis, the use of tissue adhesive remained an independent predictor for the development of incisional SSI (OR 2.77, p = 0.007).
Conclusion
The use of tissue adhesive was an independent predictor for incisional SSI following elective bariatric surgery. This is the first study to report the effects of tissue adhesive in this patient population.
Similar content being viewed by others
References
Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres A, Weiner R, Yashkov Y, Frühbeck G. International federation for surgery of obesity and metabolic disorders-European chapter (IFSO-EC); European association for the study of obesity (EASO); European association for the study of obesity management task force (EASO OMTF). Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014; 24(1):42–55.
Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–67.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity. 2013;21 Suppl 1:S1–27.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Aminian A, Jamal MH, Andalib A, et al. Is laparoscopic bariatric surgery a safe option in extremely high-risk morbidly obese patients? J Laparoendosc Adv Su Tech A. 2015;25(9):707–11.
Encinosa WE, Bernard DM, Du D, et al. Recent improvements in bariatric surgery outcomes. Med Care. 2009;47(5):531–5.
Blackburn GL, Hutter MM, Harvey AM, et al. Expert panel on weight loss surgery: executive report update. Obesity (Silver Spring). 2009;17(5):842–62.
Ban KA, Minei JP, Laronga C, et al. American College of Surgeons and Surgical Infection Society: surgical site infection guidelines, 2016 Update. J Am Coll Surg. 2017;224(1):59–74.
Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–8.
Badia JM, Casey AL, Petrosillo N, et al. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect. 2017;96(1):1–15.
Dang JT, Tran C, Switzer N, et al. Predicting surgical site infections following laparoscopic bariatric surgery: development of the BariWound tool using the MBSAQIP database. Surg Endosc. 2020;34(4):1802–11.
Shope TR, Cooney RN, McLeod J, et al. Early results after laparoscopic gastric bypass: EEA vs GIA stapled gastrojejunal anastomosis. Obes Surg. 2003;13(3):355–9.
Schauer PR, Ikramuddin S, Gourash W, et al. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–29.
Finks JF, Carlin A, Share D, et al. Effect of surgical techniques on clinical outcomes after laparoscopic gastric bypass--results from the Michigan Bariatric Surgery Collaborative. Surg Obes Relat Dis. 2011;7(3):284–9.
Shabino PJ, Khoraki J, Elegbede AF, et al. Reduction of surgical site infections after laparoscopic gastric bypass with circular stapled gastrojejunostomy. Surg Obes Relat Dis. 2016;12(1):4–9.
Chopra T, Zhao JJ, Alangaden G, et al. Preventing surgical site infections after bariatric surgery: value of perioperative antibiotic regimens. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):317–28.
Scott GR, Carson CL, Borah GL. Dermabond skin closures for bilateral reduction mammaplasties: a review of 255 consecutive cases. Plast Reconstr Surg. 2007;120(6):1460–5.
Basaran M, Kafali E, Ugurlucan M, et al. Cyanoacrylate gluing increases the effectiveness of systemic antimicrobial treatment in sternal infection: experimental study in a rodent model. Thorac Cardiovasc Surg. 2008;56(1):28–31.
Devika S, Jeyaseelan L, Sebastian G. Analysis of sparse data in logistic regression in medical research: a newer approach. J Postgrad Med. 2016;62(1):26–31.
Huemer GM, Schmidt M, Helml GH, et al. Effective wound closure with a new two-component wound closure device (Prineo™) in excisional body-contouring surgery: experience in over 200 procedures. Aesthet Plast Surg. 2012;36(2):382–6.
Kelly BD, Lundon DJ, Timlin ME, et al. Paediatric sutureless circumcision--an alternative to the standard technique. Pediatr Surg Int. 2012;28(3):305–8.
Greene D, Koch RJ, Goode RL. Efficacy of octyl-2-cyanoacrylate tissue glue in blepharoplasty. A prospective controlled study of wound-healing characteristics. Arch Facial Plast Surg. 1999;1(4):292–6.
Miller AG, Swank ML. Dermabond efficacy in total joint arthroplasty wounds. Am J Orthop (Belle Mead NJ). 2010;39(10):476–8.
Singer AJ, Quinn JV, Clark RE, et al. Closure of lacerations and incisions with octylcyanoacrylate: a multicenter randomized controlled trial. Surgery. 2002;131(3):270–6.
Switzer EF, Dinsmore RC, North Jr JH. Subcuticular closure versus Dermabond: a prospective randomized trial. Am Surg. 2003;69(5):434–6.
Freeman JT, Anderson DJ, Hartwig MG, et al. Surgical site infections following bariatric surgery in community hospitals: a weighty concern? Obes Surg. 2011;21(7):836–40.
Winfield RD, Reese S, Bochicchio K, et al. Obesity and the risk for surgical site infection in abdominal surgery. Am Surg. 2016;82(4):331–6.
Thelwall S, Harrington P, Sheridan E, et al. Impact of obesity on the risk of wound infection following surgery: results from a nationwide prospective multicentre cohort study in England. Clin Microbiol Infect. 2015;21(11):1008.e1–8.
Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999;27(2):97–132. quiz 3-4; discussion 96
Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect. 2013;14(1):73–156.
Anderson DJ, Podgorny K, Berrios-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(Suppl 2):S66–88.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fecso, A.B., Maeda, A., Duggal, S. et al. The Effect of Tissue Adhesive on Surgical Site Infection Following Elective Bariatric Surgery: a Retrospective Cohort Study. OBES SURG 31, 2988–2993 (2021). https://doi.org/10.1007/s11695-021-05332-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05332-x