Abstract
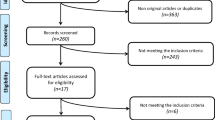
The timing of food intake throughout the day can alter circadian clocks and metabolism to modulate the course of obesity. We conducted a systematic literature review to determine whether the timing of meals could alter the change in body weight after bariatric surgery in adults. Twelve cohort studies examined the association between meal timing and changes in body weight after bariatric surgery. Eight studies suggested an association between meal timing and weight loss. All studies examined simple exposure variables such as frequency of breakfast or dinner consumption and overnight meals. Overall, the low-quality evidence that food consumption at the end of the day is associated with lower weight loss after bariatric surgery in adults warrants further research.


Similar content being viewed by others
References
Ramos A, Kow L, Fracs B, et al. IFSO & dendrite clinical systems. :100.
Velapati SR, Shah M, Kuchkuntla AR, et al. Weight regain after bariatric surgery: prevalence, etiology, and treatment. Curr Nutr Rep. 2018;7(4):329–34.
King WC, Hinerman AS, Belle SH, et al. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320(15):1560–9.
Mann JP, Jakes AD, Hayden JD, et al. Systematic review of definitions of failure in revisional bariatric surgery. Obes Surg. 2015;25(3):571–4.
Sudlow AC, le Roux CW, Pournaras DJ. Review of advances in anti-obesity pharmacotherapy: implications for a multimodal treatment approach with metabolic surgery. Obes Surg. 2019;29(12):4095–104.
Srivastava G, Buffington C. A specialized medical management program to address post-operative weight regain in bariatric patients. Obes Surg. 2018;28(8):2241–6.
Thorell A, MacCormick AD, Awad S, et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg. 2016;40(9):2065–83.
Chaix A, Manoogian ENC, Melkani GC, et al. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu Rev Nutr. 2019;39:291–315.
Hatori M, Vollmers C, Zarrinpar A, et al. Time-restricted feeding without reducing caloric intake prevents metabolic diseases in mice fed a high-fat diet. Cell Metab. 2012;15(6):848–60.
Garaulet M, Gómez-Abellán P, Alburquerque-Béjar JJ, et al. Timing of food intake predicts weight loss effectiveness. Int J Obes. 2013;37(4):604–11.
McHill AW, Phillips AJ, Czeisler CA, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106(5):1213–9.
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22(5):789–98.
Wilkinson MJ, Manoogian ENC, Zadourian A, et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 2019;31(1):92–104.
Lowe DA, Wu N, Rohdin-Bibby L, et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT Randomized Clinical Trial. JAMA Intern Med. 2020;180(11):1–9.
Cienfuegos S, Gabel K, Kalam F, et al. Effects of 4- and 6-h Time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 2020;32(3):366–78.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Booth A, Clarke M, Dooley G, et al. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2.
Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Ruiz-Lozano T, Vidal J, de Hollanda A, et al. Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin Nutr. 2016;35(6):1308–14.
Ruiz-Lozano T, Vidal J, de Hollanda A, et al. Evening chronotype associates with obesity in severely obese subjects: interaction with CLOCK 3111T/C. Int J Obes. 2016;40(10):1550–7.
Bergh I, Lundin Kvalem I, Risstad H, et al. Preoperative predictors of adherence to dietary and physical activity recommendations and weight loss one year after surgery. Surg Obes Relat Dis. 2016;12(4):910–8.
Masood A, Alsheddi L, Alfayadh L, et al. Dietary and lifestyle factors serve as predictors of successful weight loss maintenance postbariatric surgery. J Obes. 2019;2019:7295978.
Unal S, Sevincer GM, Maner AF. Prediction of weight regain after bariatric surgery by night eating, emotional eating, eating concerns, depression and demographic characteristics. Turk J Psychiatry. 2019;30(1):31–41.
Sioka E, Tzovaras G, Oikonomou K, et al. Influence of eating profile on the outcome of laparoscopic sleeve gastrectomy. Obes Surg. 2013;23(4):501–8.
Ferreira Pinto T, Carvalhedo de Bruin PF, Sales de Bruin VM, et al. Effects of bariatric surgery on night eating and depressive symptoms: a prospective study. Surg Obes Relat Dis. 2017;13(6):1057–62.
Ivezaj V, Kessler EE, Lydecker JA, et al. Loss-of-control eating following sleeve gastrectomy surgery. Surg Obes Relat Dis. 2017;13(3):392–8.
Ames GE, Heckman MG, Diehl NN, et al. Guiding patients toward the appropriate surgical treatment for obesity: should presurgery psychological correlates influence choice between Roux-en-Y gastric bypass and vertical sleeve gastrectomy? Obes Surg. 2017;27(10):2759–67.
Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016;49(12):1058–67.
Papalazarou A, Yannakoulia M, Kavouras SA, et al. Lifestyle intervention favorably affects weight loss and maintenance following obesity surgery. Obesity (Silver Spring). 2010;18(7):1348–53.
Colles SL, Dixon JB, O’Brien PE. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity (Silver Spring). 2008;16(3):615–22.
Gluck ME, Venti CA, Salbe AD, et al. Nighttime eating: commonly observed and related to weight gain in an inpatient food intake study. Am J Clin Nutr. 2008;88(4):900–5.
Xiao Q, Garaulet M, Scheer FAJL. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43(9):1701–11.
Root TL, Thornton LM, Lindroos AK, et al. Shared and unique genetic and environmental influences on binge eating and night eating: a Swedish twin study. Eat Behav. 2010;11(2):92–8.
De Zwaan M, Marschollek M, Allison KC. The night eating syndrome (NES) in bariatric surgery patients. Eur Eat Disord Rev. 2015;23(6):426–34.
Yoshida J, Eguchi E, Nagaoka K, et al. Association of night eating habits with metabolic syndrome and its components: a longitudinal study. BMC Public Health. 2018;18(1):1366.
Gupta NJ, Kumar V, Panda S. A camera-phone based study reveals erratic eating pattern and disrupted daily eating-fasting cycle among adults in India. PLoS One. 2017;12(3):e0172852.
Qin L-Q, Li J, Wang Y, et al. The effects of nocturnal life on endocrine circadian patterns in healthy adults. Life Sci. 2003;73(19):2467–75.
Hibi M, Masumoto A, Naito Y, et al. Nighttime snacking reduces whole body fat oxidation and increases LDL cholesterol in healthy young women. Am J Phys Regul Integr Comp Phys. 2013;304(2):R94–101.
Bandín C, Scheer FAJL, Luque AJ, et al. Meal timing affects glucose tolerance, substrate oxidation and circadian-related variables: a randomized, crossover trial. Int J Obes. 2015;39(5):828–33.
Bo S, Fadda M, Castiglione A, et al. Is the timing of caloric intake associated with variation in diet-induced thermogenesis and in the metabolic pattern? A randomized cross-over study. Int J Obes. 2015;39(12):1689–95.
Collado MC, Engen PA, Bandín C, et al. Timing of food intake impacts daily rhythms of human salivary microbiota: a randomized, crossover study. FASEB J. 2018;32(4):2060–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed Consent
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 288 kb).
Rights and permissions
About this article
Cite this article
Cossec, M., Atger, F., Blanchard, C. et al. Daily Timing of Meals and Weight Loss After Bariatric Surgery: a Systematic Review. OBES SURG 31, 2268–2277 (2021). https://doi.org/10.1007/s11695-021-05278-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05278-0