Abstract
Background
Cardiovascular disease (CVD) is highly prevalent in obese patients and is the leading cause of death. High levels of plasma low-density lipoprotein cholesterol (LDL-C) are associated with higher coronary artery disease (CAD) risk. The aim of the study was to assess the impact of the Roux-en-Y gastric bypass on the achievement of the currently proposed cardiovascular prevention goals after 1 year.
Patients and Methods
We performed a retrospective analysis from a prospectively built database of patients who underwent a primary Roux-en-Y gastric bypass (RYGB) from 2004 to 2018. Patients with intermediate, high, or very high risk for CVD according to the 2018 AHA/ACC or the 2019 ESC/EAS guidelines were selected. An analysis of clinical and biochemical variables in 1 year was performed. Logistic multivariate regressions were made to assess the impact of preoperative and weight loss parameters in the achievement of LDL-C goals.
Results
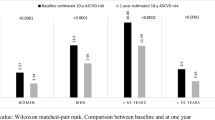
From 1039 patients, 70 met the selection criteria and were included in the analysis of the 2018 AHA/ACC guidelines, and 75 in the 2019 ESC/EAS guidelines. Mean decrease in LDL-C levels was 21.1 ± 40.2 mg/dL 1 year after surgery, and 29/34 patients were off medications. The percentage of patients achieving LDL-C goals according to the 2018 AHA/ACC guidelines was 27.1%, whereas according to the 2019 ESC/EAS guidelines, the percentages was 9.3%. The %TWL was associated with achieving LDL-C goals according to the 2018 AHA/ACC at 1 year.
Conclusions
RYGB induces a significant weight loss and an improvement in LDL-C levels 1 year after surgery. The number of patients that reached the goals varies according to the guidelines used and ranged from 9.3 to 27.1%.




Similar content being viewed by others
Abbreviations
- AACE:
-
America Association of Clinical Endocrinologists
- ACC:
-
American College of Cardiology
- AHA:
-
American Heart Association
- ASCVD:
-
Atherosclerotic Cardiovascular Disease
- ASMBS:
-
American Society for Metabolic and Bariatric Surgery
- BMI:
-
Body mass index
- BPD:
-
Biliopancreatic diversion
- CAD:
-
Coronary artery disease
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- EAS:
-
European Atherosclerosis Society
- ESC:
-
European Society of Cardiology
- EWL:
-
Excess of weight loss
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- OAGB:
-
One-anastomosis gastric bypass
- PIB:
-
Partial ileal bypass
- RYGB:
-
Roux-en-Y gastric bypass
- SG:
-
Sleeve gastrectomy
- T2D:
-
Type 2 diabetes
- TC:
-
Total cholesterol
- TWL:
-
Total weight loss
References
Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016. Geneva, World Health Organization; 2018. https://www.who.int/healthinfo/global_burden_disease/estimates/en/.
Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170 000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. J Am Coll Cardiol. 2019;73(24):e285–350.
Nguyen NT, Varela E, Sabio A, et al. Resolution of hyperlipidemia after laparoscopic Roux-en-Y gastric bypass. J Am Coll Surg. 2006;203(1):24–9.
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. ESC Scientific DocumentGroup. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;1;41(1):111–188. https://doi.org/10.1093/eurheartj/ehz455.
Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98(24):1763–77.
Puzziferri N, Roshek TB, Mayo HG, et al. Long-term follow-up after bariatric surgery. JAMA. 2014;312(9):934–42.
Zambon S, Romanato G, Sartore G, et al. Bariatric surgery improves atherogenic LDL profile by triglyceride reduction. Obes Surg. 2009;19(2):190–5.
Campos C, Matts J, Fitch L, et al. Lipoprotein modification achieved by partial ileal bypass: five-year results of the Program on the Surgical Control of the Hyperlipidemias. Surgery. 1987;102(2):424–32.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–91.
Busetto L, Dicker D, Azran C, et al. Practical recommendations of the Obesity Management Task Force of the European Association for the study of obesity for the post-bariatric surgery medical management. Obes Facts. 2017;10(6):597–632.
Blanco DG, Funes DR, Giambartolomei G, et al. High cardiovascular risk patients benefit more from bariatric surgery than low cardiovascular risk patients. Surg Endosc. 2019;33(5):1626–31.
Cholesterol Treatment Trialists’ (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380(9841):581–90.
Buchwald H, Bourdages HR, Campos CT, et al. Impact of cholesterol reduction on peripheral arterial disease in the Program on the Surgical Control of the Hyperlipidemias (POSCH). Surgery. 1996;120(4):672–9.
Buchwald H, Rudser KD, Williams SE, et al. Overall mortality, incremental life expectancy, and cause of death at 25 years in the Program on the Surgical Control of the Hyperlipidemias. Ann Surg. 2010;251(6):1034–40.
Buchwald H, Varco R, Boen JR. Effective lipid modification by partial ileal bypass reduced long-term coronary heart disease mortality and morbidity: five-year posttrial follow-up report from the POSCH. Arch Intern Med. 1998;158(11):1253–61.
de Dios García-Díaz J, Lozano O, Ramos JC, et al. Changes in lipid profile after biliopancreatic diversion. Obes Surg. 2003;13(5):756–60.
Milone M, Lupoli R, Maietta P, et al. Lipid profile changes in patients undergoing bariatric surgery: a comparative study between sleeve gastrectomy and mini-gastric bypass. Int J Surg. 2015;14:28–32.
Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Bagheri MJ, Talebpour M, Sharifi A, Talebpour A, Mohseni A. Lipid profile change after bariatric surgeries: laparoscopic gastric plication versus mini gastric bypass. Acta Chir Belg. 2019;119(3):146–51. https://doi.org/10.1080/00015458.2018.1479022.
American Diabetes Association. Cardiovascular disease and risk management: standards of medical care in diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S103–23.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The institutional review board approved this study. This article does not contain any studies with human participants or animals performed by any of the authors.
Consent Statements
Non-applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ponce de León-Ballesteros, G., Sánchez-Aguilar, H.A., Aguilar-Salinas, C.A. et al. Reaching LDL-C Targets in Patients with Moderate, High, and Very High Risk for Cardiovascular Disease After Bariatric Surgery According to Different Guidelines. OBES SURG 31, 2087–2096 (2021). https://doi.org/10.1007/s11695-021-05221-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-021-05221-3