Abstract
Background
Visceral Adiposity Index (VAI) is considered to be a reliable indicator for evaluation of visceral adipose dysfunction and cardiovascular disease risk. However, no previous studies have reported the VAI variation after bariatric surgery and the predictive effect of preoperative VAI on diabetes remission. The aim of this study is to evaluate whether preoperative VAI is useful to predict diabetes remission in low BMI Chinese patients after bariatric surgery.
Methods
Eighty-seven type 2 diabetes mellitus patients with BMI < 35 kg/m2 underwent bariatric surgery from May 2010 to March 2018 in our hospital. VAI, glycolipid metabolic parameters, and anthropometric variables were measured before and 4 years after surgery. Complete remission was defined as follows: HbA1c < 6%, FPG < 5.6 mmol/L, achieved without anti-diabetic medication. Analysis included using binary logistic regression to identify predictors and ROC curves to determine clinically useful cutoff values.
Results
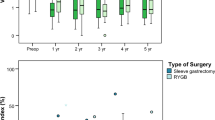
Seventy-four patients (85.1%) underwent Roux-en-Y gastric bypass (RYGB), while the remaining 13 patients (14.9%) underwent sleeve gastrectomy (SG). Patients’ weight, glycemic control, and lipid profiles were improved significantly after surgery (p < 0.05). Complete remission of T2DM was found in 35 patients (40.2%) 1 year after surgery. VAI decreased from baseline 4.41 to 1.74 in 3 months after surgery (p < 0.05) and showed a downward trend over the period from 6 months to 4 years. Patients with complete remission had a significantly shorter duration of diabetes, lower HbA1c level, and higher VAI, in comparison to those without remission. Binary logistics regression and ROC curves analysis confirm that VAI, HbA1c, and duration of diabetes can predict diabetes remission after bariatric surgery, and the VAI of 4.46 is a useful threshold for predicting surgical efficacy.
Conclusion
VAI is a significant predictor of diabetes remission for lower BMI patients with T2DM following bariatric surgery in China. The VAI of 4.46 is a useful threshold for predicting surgical efficacy. Multi-center and larger prospective studies are needed to confirm our findings.


Similar content being viewed by others
References
Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Adams TD, Arterburn DE, Nathan DM, et al. Clinical outcomes of metabolic surgery: microvascular and macrovascular complications. Diabetes Care. 2016;39(6):912–23.
Dixon JB, Zimmet P, Alberti KG, et al. Bariatric surgery: an IDF statement for obese type 2 diabetes. Arq Bras Endocrinol Metabol. 2011;55(6):367–82.
Xu Y, Wang L, He J, et al. Prevalence and control of diabetes in Chinese adults. JAMA. 2013;310(9):948–59.
Batterham RL, Cummings DE. Mechanisms of diabetes improvement following bariatric/metabolic surgery. Diabetes Care. 2016;39(6):893–901.
Albaugh VL, Banan B, Antoun J, et al. Role of bile acids and GLP-1 in mediating the metabolic improvements of bariatric surgery. Gastroenterology. 2019;156(4):1041–51. e4
Liu H, Hu C, Zhang X, et al. Role of gut microbiota, bile acids and their cross-talk in the effects of bariatric surgery on obesity and type 2 diabetes. J Diabetes Investig. 2018;9(1):13–20.
Ji G, Li P, Li W, et al. The effect of bariatric surgery on Asian patients with type 2 diabetes mellitus and body mass index < 30 kg/m(2): a systematic review and meta-analysis. Obes Surg. 2019;29(8):2492–502.
Sha Y, Huang X, Ke P, et al. Laparoscopic Roux-en-Y gastric bypass versus sleeve gastrectomy for type 2 diabetes mellitus in nonseverely obese patients: a systematic review and meta-analysis of randomized controlled trials. Obes Surg. 2020;30(5):1660–70.
Baskota A, Li S, Dhakal N, et al. Bariatric surgery for type 2 diabetes mellitus in patients with BMI <30 kg/m2: a systematic review and meta-analysis. PLoS One. 2015;10(7):e0132335.
Wang GF, Yan YX, Xu N, et al. Predictive factors of type 2 diabetes mellitus remission following bariatric surgery: a meta-analysis. Obes Surg. 2015;25(2):199–208.
Lee WJ, Chong K, Chen SC, et al. Preoperative prediction of type 2 diabetes remission after gastric bypass surgery: a comparison of DiaRem scores and ABCD scores. Obes Surg. 2016;26(10):2418–24.
Yu HY et al. Visceral fat area as a new predictor of short-term diabetes remission after Roux-en-Y gastric bypass surgery in Chinese patients with a body mass index less than 35 kg/m(2). Surg Obes Relat Dis. 2015;11(1):6–13.
Amato MC, Giordano C, Galia M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33(4):920–2.
Randrianarisoa E, Lehn-Stefan A, Hieronimus A, et al. Visceral Adiposity Index as an independent marker of subclinical atherosclerosis in individuals prone to diabetes mellitus. J Atheroscler Thromb. 2019;26(9):821–34.
Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375(9712):408–18.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Bray GA, Heisel WE, Afshin A, et al. The science of obesity management: an Endocrine Society scientific statement. Endocr Rev. 2018;39(2):79–132.
Wang C, Zhang H, Yu H, et al. Roux-en-Y gastric bypass for T2D treatment in Chinese patients with low BMI: 5-year outcomes. Obes Surg. 2020;30:2588–97.
Mingrone G, Panunzi S, de Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386(9997):964–73.
Pournaras DJ, le Roux CW. Type 2 diabetes: multimodal treatment of a complex disease. Lancet. 2015;386(9997):936–7.
Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–52.
Yusuf S, Hawken S, Ôunpuu S, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366(9497):1640–9.
Shuster A, Patlas M, Pinthus JH, et al. The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br J Radiol. 2012;85(1009):1–10.
Amato MC, Giordano C. Visceral Adiposity Index: an indicator of adipose tissue dysfunction. Int J Endocrinol. 2014;2014:730827.
Baloglu I et al. The relationship between Visceral Adiposity Index and epicardial adipose tissue in patients with type 2 diabetes mellitus. Exp Clin Endocrinol Diabetes. 2019;
Nusrianto R, Ayundini G, Kristanti M, et al. Visceral Adiposity Index and lipid accumulation product as a predictor of type 2 diabetes mellitus: the Bogor cohort study of non-communicable diseases risk factors. Diabetes Res Clin Pract. 2019;155:107798.
Kouli GM, Panagiotakos DB, Kyrou I, et al. Visceral Adiposity Index and 10-year cardiovascular disease incidence: the ATTICA study. Nutr Metab Cardiovasc Dis. 2017;27(10):881–9.
Derezinski T et al. Visceral Adiposity Index as a useful tool for the assessment of cardiometabolic disease risk in women aged 65 to 74. Diabetes Metab Res Rev. 2018;34(8):e3052.
Lee WJ, Almulaifi A, Chong K, et al. The effect and predictive score of gastric bypass and sleeve gastrectomy on type 2 diabetes mellitus patients with BMI < 30 kg/m(2). Obes Surg. 2015;25(10):1772–8.
Yan W et al. Preoperative fasting plasma C-peptide levels as predictors of remission of type 2 diabetes mellitus after bariatric surgery: a systematic review and meta-analysis. J Investig Surg. 2017:1–11.
Hsu CC, Almulaifi A, Chen JC, et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: five-year outcomes. JAMA Surg. 2015;150(12):1117–24.
Aminian A, Andalib A, Khorgami Z, et al. A nationwide safety analysis of bariatric surgery in nonseverely obese patients with type 2 diabetes. Surg Obes Relat Dis. 2016;12(6):1163–70.
Du X et al. A comparative study of the metabolic effects of LSG and LRYGB in Chinese diabetes patients with BMI<35 kg/m(2). Surg Obes Relat Dis. 2017;13(2):189–97.
Ke Z, Li F, Chen J, et al. Effects of laparoscopic Roux-en-Y gastric bypass for type 2 diabetes mellitus: comparison of BMI > 30 and < 30 kg/m2. Obes Surg. 2017;27:3040–7.
Voglino C, Tirone A, Ciuoli C, et al. Cardiovascular benefits and lipid profile changes 5 years after bariatric surgery: a comparative study between sleeve gastrectomy and Roux-en-Y gastric bypass. J Gastrointest Surg. 2019;
Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26(11):2590–601.
Acknowledgments
We thank Ms. Liying Wang and Ms. Yiming Chai for the hard work of English editing and polishing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Statement of Human Rights
The study was approved by the Ethics Committee of Army Medical University Affiliated Daping Hospital and complied with the Declaration of Helsinki.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ke, Z., Li, F., Gao, Y. et al. The Use of Visceral Adiposity Index to Predict Diabetes Remission in Low BMI Chinese Patients After Bariatric Surgery. OBES SURG 31, 805–812 (2021). https://doi.org/10.1007/s11695-020-05034-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05034-w