Abstract
Introduction
Bariatric surgery is a first-line treatment for patients with obesity and diabetes. It is uncertain whether leptin has an influence on glycemia in the postoperative period.
Methods
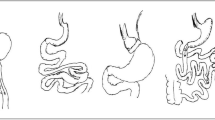
A cohort study of thirty-eight individuals with obesity and diabetes who underwent laparoscopic Roux-en-Y gastric bypass was undertaken. The levels of leptin, glucose, and glycosylated hemoglobin were verified in the preoperative period and in the first and third postoperative months.
Results
The majority of patients were women (81.6%), and the mean age was 47.3 years (SD 8.8). The mean BMI was reduced by 17.75% (from 47.3 to 38.9 kg/m2) and the mean glycemia by 26.76%. Preoperative leptin had a moderate positive correlation with glucose level at the third month (Pearson r = 0.46, P = 0.02), but not with HbA1c. Patients with leptin above 27.34 ng/mL had a higher glucose level at the end of observation (101.9 versus 88.9, t test, P = 0.042).
Conclusion
The search for factors that influence diabetes control after bariatric surgery is of major importance in clinical practice. Our study reported a level of leptin that can predict the prognosis of glycemic control after the intervention. This finding still needs to be validated and confirmed in other populations.

Similar content being viewed by others
References
Twig G, Afek A, Derazne E, et al. Diabetes risk among overweight and obese metabolically healthy young adults. Diabetes Care. 2014;37(11):2989–95.
Guraya SY, Strate T. Surgical outcome of laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass for resolution of type 2 diabetes mellitus: a systematic review and meta-analysis. World J Gastroenterol. 2020;26(8):865–76.
Mechanick JI et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic and Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Obesity (Silver Spring). 2020;28(4):O1–O58.
Salman MA, el-Ghobary M, Soliman A, et al. Long-term changes in leptin, chemerin, and ghrelin levels following Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Obes Surg. 2020;30(3):1052–60.
Maffei M, Halaas J, Ravussin E, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med. 1995;1(11):1155–61.
Frederich RC, Hamann A, Anderson S, et al. Leptin levels reflect body lipid content in mice: evidence for diet-induced resistance to leptin action. Nat Med. 1995;1(12):1311–4.
Morton GJ. Hypothalamic leptin regulation of energy homeostasis and glucose metabolism. J Physiol. 2007;583(Pt 2):437–43.
El-Haschimi K et al. Two defects contribute to hypothalamic leptin resistance in mice with diet-induced obesity. J Clin Invest. 2000;105(12):1827–32.
D'souza AM, Neumann UH, Glavas MM, et al. The glucoregulatory actions of leptin. Mol Metab. 2017;6(9):1052–65.
Mokadem M, Zechner JF, Uchida A, et al. Leptin is required for glucose homeostasis after Roux-en-Y gastric bypass in mice. PLoS One. 2015;10(10):e0139960.
Standards of medical care in diabetes-2017: summary of revisions. Diabetes Care. 2017;40(Suppl 1):S4–5.
Kleiner DE, Brunt EM. Nonalcoholic fatty liver disease: pathologic patterns and biopsy evaluation in clinical research. Semin Liver Dis. 2012;32(1):3–13.
Lindegaard KK, Jorgensen NB, Just R, et al. Effects of Roux-en-Y gastric bypass on fasting and postprandial inflammation-related parameters in obese subjects with normal glucose tolerance and in obese subjects with type 2 diabetes. Diabetol Metab Syndr. 2015;7:12.
Zhao S et al. Partial leptin reduction as an insulin sensitization and weight loss strategy. Cell Metab. 2019;30(4):706–719.e6.
Liu W, Zhou X, Li Y, et al. Serum leptin, resistin, and adiponectin levels in obese and non-obese patients with newly diagnosed type 2 diabetes mellitus: a population-based study. Medicine (Baltimore). 2020;99(6):e19052.
Min T, Prior SL, Dunseath G, et al. Temporal effects of bariatric surgery on adipokines, inflammation and oxidative stress in subjects with impaired glucose homeostasis at 4 years of follow-up. Obes Surg. 2020;30(5):1712–8.
Engin AB. Adipocyte-macrophage cross-talk in obesity. Adv Exp Med Biol. 2017;960:327–43.
Liberale L, Bonaventura A, Carbone F, et al. Early reduction of matrix metalloproteinase-8 serum levels is associated with leptin drop and predicts diabetes remission after bariatric surgery. Int J Cardiol. 2017;245:257–62.
Khosravi-Largani M, Nojomi M, Aghili R, et al. Evaluation of all types of metabolic bariatric surgery and its consequences: a systematic review and meta-analysis. Obes Surg. 2019;29(2):651–90.
Lee Y et al. Complete resolution of nonalcoholic fatty liver disease after bariatric surgery: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2019;17(6):1040–1060.e11.
Souto KP, Meinhardt NG, Ramos MJ, et al. Nonalcoholic fatty liver disease in patients with different baseline glucose status undergoing bariatric surgery: analysis of intraoperative liver biopsies and literature review. Surg Obes Relat Dis. 2018;14(1):66–73.
Burza MA, Romeo S, Kotronen A, et al. Long-term effect of bariatric surgery on liver enzymes in the Swedish Obese Subjects (SOS) study. PLoS One. 2013;8(3):e60495.
Rosenbaum M et al. Effects of gender, body composition, and menopause on plasma concentrations of leptin. J Clin Endocrinol Metab. 1996;81(9):3424–7.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human and Animal Rights/Ethical Approval
The study was approved by the HCPA Ethical Committee number 1,959,671. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cabrera, L.O., Trindade, E.N., Leite, C. et al. Preoperative Level of Leptin Can Be a Predictor of Glycemic Control for Patients with Diabetes Undergoing Bariatric Surgery. OBES SURG 30, 4829–4833 (2020). https://doi.org/10.1007/s11695-020-05011-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-05011-3