Abstract
Background
Obesity and type 2 diabetes mellitus (T2DM) represent significant healthcare burdens. Surgical management is superior to traditional medical therapy. Laparoscopic sleeve gastrectomy (LSG) and gastric bypass (both Roux-en-Y (RYGB) and one anastomosis gastric bypass (OAGB) are the most commonly performed metabolic procedures. It remains unclear which gives the optimal quality-of-life pay-off in the context of T2DM. This study compares LSG, RYGB, and OAGB in the management of T2DM and obesity using modeled decision analysis. Alternative approaches were assessed considering efficacy of interventions, post-operative complications, and quality of life outcomes to determine the optimal approach.
Methods
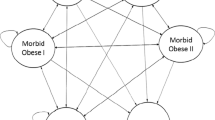
Modeled decision analysis was performed from the patent’s perspective comparing best medical management (MM), SG, RYGB, OAGB, and LAGB. The base case is a 40-year-old female with a body mass index (BMI) of 40 and T2DM. Input variables were calculated based on published decision analyses and a literature review. Utilities were based on previous studies. Sensitivity analysis was performed. The payoff was quality-adjusted life years (QALYs) 5 years from intervention. TreeAge Pro modeling software was used for analysis.
Results
In 5-years post-procedure, OAGB gave the optimal QALY payoff of 3.65 QALYs (reviewer 2). RYGB gave 3.47, SG gave 3.08, LAGB gave 2.62 and MM 2.45 QALYs. Three input variables proved sensitive. RYGB is optimal if its metabolic improvement rates exceed 86%. It is also optimal if metabolic improvement rates in OAGB drop below 71.8% or if the utility of OAGB drops below 0.759.
Conclusion
OAGB gives the optimal QALY payoff in treatment of T2DM. RYGB and SG also improve metabolic outcomes and remain viable options in selected patients.




Similar content being viewed by others
References
Association AD. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(1):62–9.
Zheng Y, Ley SH, FB H. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14:88–98.
Bommer C, Heesemann E, Sagalova V, et al. The global economic burden of diabetes in adults aged 20-79 years: a cost-of-illness study. Lancet Diabetes Endocrinol. 2017;5:423–30.
Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41:963–70.
Roper NA, Bilous RW, Kelly WF, et al. Excess mortality in a population with diabetes and the impact of material deprivation: longitudinal, population based study. Bmj. 2001;322:1389–93.
Norris SL, Xhang X, Avenell A, et al. Pharmacotherapy for weight loss in adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;1:CD004096.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes- 5-year outcomes. N Engl J Med. 2017;376:641–51.
Buchwald H, DM O. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–36.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial- a prospective controlled intervention study of bariatric study. J Intern Med. 2013;273:219–34.
Brethauer SA, Aminian A, Romero-Talamas H, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258:628–36.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database System Rev. 2014;2014:CD003641.
Rubino F, Nathan DM, Eckel RH, et al. Metabolic surgery in the treatment algorithm for type 2 diabetes: a joint statement by international diabetes organizations. Surg Obes Relat Dis. 2016;12:1144–62.
Ramos A, Kow L, Brown W, Welbourn R, Dixon J, Kinsman R, et al. 5th IFSO global registry report 2019. The International Federation for the Surgery of Obesity and Metabolic Disorders.; 2019.
English WJ, DeMaria EJ, Hutter MM, et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. 2020;16(4):457–63.
Rutledge R. The Mini-Gastric Bypass: Experience with the first 1,274 cases. Obes Surg. 2001;11:276–80.
Mahawar K, Himpens J, Shikora S, et al. The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28:303–12.
Keogh S, Bolger JC, Brady S, et al. Options in bariatric surgery: modeled decision analysis supports roux-en-Y gastric bypass and sleeve gastrectomy as the treatments of choice. Surg Obes Relat Dis. 2018;14:1670–7.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.
Merz AE, Blackstone RB, Gagner M, et al. Duodenal switch in revisional bariatric surgery: conclusions from an expert consensus panel. Surg Obes Relat Dis. 2019;15:894–9.
Risstad H, Sovik T, Engstrom M, et al. Five-year outcomes after laparoscopic gastric bypass and laparoscopic duodenal switch in patients with body mass index of 50 to 60: a randomized clinical trial. JAMA Surg. 2015;150:352–61.
Bolckmans R. J H. long-term (<10 years) outcome of the laparoscopic biliopancreatic diversion with duodenal switch. Ann Surg. 2016;264:1029–37.
Demaria EJ, Winegar DA, Pate VW, et al. Postoperative outcomes of metabolic surgery to treat diabetes participating in the ASMBS bariatric surgery center of excellence program as reported in the bariatric outcomes longitudinal database. Ann Surg. 2010;252:559–66.
Detsky AS, Naglie G, Krahn MD, et al. Primer on medical decision analysis: part 1— getting started. Med Decis Mak. 1997;17:123–5.
Detsky AS, Naglie G, Krahn MD, et al. Primer on medical decision analysis: Part 2— Building a tree. Med Decis Mak. 1997;17:126–35.
Krahn MD, Naglie G, Naimark D, et al. Primer on medical decision analysis: part 4— analyzing the model and interpreting the results. Med Decis Mak. 1997;17:142–51.
Naglie G, Krahn MD, Naimark D, et al. Primer on medical decision analysis: part 3— estimating probabilities and utilities. Med Decis Mak. 1997;17:136–41.
Naimark D, Krahn MD, Naglie G, et al. Primer on medical decision analysis: part 5— working with Markov processes. Med Decis Mak. 1997;17:152–9.
Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey 2016: primary, Endoluminal, and Revisional procedures. Obes Surg. 2018;28:3873–794.
Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100.
Arterburn DE, Bogart A, Sherwood NE, et al. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obes Surg. 2013;23:93–102.
Lee WJ, Chong K, Lin YH, et al. Laparoscopic sleeve gastrectomy versus single anastomosis (mini-) gastric bypass for the treatment of type 2 diabetes mellitus: 5-year results of a randomized trial and study of incretin effect. Obes Surg. 2014;24:1552–62.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28:156–63.
Zhang Y, Zhao H, Cao Z, et al. A randomized clinical trial of laparoscopic roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg. 2014;24:1617–24.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5-year follow-up of an open-label, single-Centre, randomised controlled trial. Lancet. 2015;386:964–73.
Hsu CC, Almulafi A, Chen JC, et al. Effect of bariatric surgery vs medical treatment on type 2 diabetes in patients with body mass index lower than 35: five-year outcomes. JAMA Surg. 2015;150:1117–24.
Bruzzi M, Rau C, Voron T, et al. Single anastomosis or mini-gastric bypass: long-term results and quality of life after a 5-ear follow-up. Surg Obes Relat Dis. 2015;11(2):321–6.
Gulliford MC, Booth HP, Reddy M, et al. Effect of contemporary bariatric surgical procedures on type 2 diabetes remission. A population-based matched cohort study. Obes Surg. 2016;26:2308–15.
Dicker D, Yahalom R, Comaneshter DS, et al. Long-term outcomes of three types of bariatric surgery on obesity and type 2 diabetes control and remission. Obes Surg. 2016;26:1814–20.
Wentworth JM, Burton P, Laurie C, et al. Five-year outcomes of a randomized trial of gastric band surgery in overweight but not obese people with type 2 diabetes. Diabetes Care. 2017;40:e44–5.
Ikramuddin S, Korner J, Lee WJ, et al. Lifestyle intervention and medical management with vs without roux-en-Y gastric bypass and control of hemoglobin A1c, LDL cholesterol, and systolic blood pressure at 5 years in the diabetes surgery study. JAMA Surg. 2018;319:266–78.
Salminen P, Helmio M, O’vaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg. 2018;319:241–54.
Peterli R, Wolnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA Surg. 2018;265:466–73.
Ruiz-Tovar J, Carbajo MA, Jiminez JM, et al. Long-term follow-up after sleeve gastrectomy versus Roux-en-Y gastric bypass versus one-anastomosis gastric bypass: a prospective randomized comparative study of weight loss and remission of comorbidities. Surg Endosc. 2019;33:401–10.
Bolger JC, Kelly ME, Barry K. Acute appendicitis in the adult population: Modelled decision analysis supports a conservative approach. J Gastrointest Surg. 2015;19:2249–57.
Campos GM, Khoraki J, Browning MG, et al. Changes in utilization of bariatric surgery in the United States from 1993–2016. Ann Surg. 2019;271:201–9.
Eliasson B, Liakopoulos V, Franzen S, et al. Cardiovascular disease and mortality in patients with type 2 diabetes after bariatric surgery in Sweden: a nationwide, matched, observational cohort study. Lancet Diabetes Endocrinol. 2015;3:847–54.
Johnson BL, Blackhurst DW, Latham BB, et al. Bariatric surgery is associated with a reduction in major macrovascular and microvascular complications in moderately to severly obese patients with type 2 diabetes mellitus. J Am Coll Surg. 2013;216:545–56.
Lee WJ, Ser KH, Tsou JJ, et al. Laparoscopic roux-en-Y vs mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22:1827–34.
Fisher BL, Buchwald H, Clark W, et al. Mini-gastric bypass controversy. Obes Surg. 2001;11:773–7.
Magouliotis DE, Tasiopoulou VS, Tzovaras G. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for morbid obesity: an updated meta-analysis. Obes Surg. 2019;29:2721–30.
Sebastianelli L, Benois M, Vanbiervliet G, et al. Systematic endoscopy 5 years after sleeve gastrectomy results in a high rate of Barrett’s esophagus: results of a multicentre study. Obes Surg. 2019;29:1462–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All the above authors declare no conflict of interest.
Ethical Approval
For this type of study formal consent is not required.
Informed Consent
Does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brosnan, C., Bolger, J.C., Bolger, E.M. et al. Options in Bariatric Surgery: Modeled Decision Analysis Supports One-Anastomosis Gastric Bypass as the Treatment of Choice when Type 2 Diabetes Is Present. OBES SURG 30, 5001–5011 (2020). https://doi.org/10.1007/s11695-020-04921-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04921-6