Abstract
Purpose
Physical activity, sedentary behavior, and sleep have been linked to the likelihood of maintaining healthy body weight. This study aimed to determine objectively measured movement behaviors before and up to 18 months after bariatric surgery and to investigate whether preoperative levels of these movement behaviors and potential changes of these behaviors were associated with changes in body weight and boy composition.
Materials and Methods
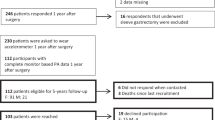
Accelerometer determined total physical activity, moderate-to-vigorous physical activity (MVPA), light physical activity, sedentary behavior, and sleep (for six consecutive days and seven nights) were assessed approximately 3 months and 1–2 weeks before surgery as well as 6 and 18 months after surgery (n = 41). Body weight and body composition (waist circumference, fat mass, and fat-free mass) were determined at each visit.
Results
Mean weight loss 18 months after surgery was 42.0 ± 1.9 kg. There were no pre- to postoperative improvements in physical activity, sedentary behavior, or sleep. However, greater increases in levels of total physical activity and time spent in MVPA from 3 months before to 6 months after surgery predicted better weight loss and larger reductions in fat mass and waist circumference. Unexpectedly, a lower level of physical activity and a higher level of sedentary behavior before surgery predicted better weight loss outcomes.
Conclusion
Objectively measured movement behaviors do not improve after bariatric surgery despite a substantial weight loss. However, increasing total physical activity and/or more time spent in MVPA after surgery may increase weight loss and lead to favorable changes in body composition.
Similar content being viewed by others
Change history
02 December 2020
A Correction to this paper has been published: <ExternalRef><RefSource>https://doi.org/10.1007/s11695-020-05137-4</RefSource><RefTarget Address="10.1007/s11695-020-05137-4" TargetType="DOI"/></ExternalRef>
References
Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–55.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet. 2015;386:964–73.
Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity. JAMA. 2018;319:255–65.
Corcelles R, Boules M, Froylich D, et al. Total weight loss as the outcome measure of choice after Roux-en-Y gastric bypass. Obes Surg. 2016;26:1794–8.
Lutfi R, Torquati A, Sekhar N, et al. Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc. 2006;20:864–7.
Campos GM, Rabl C, Mulligan K, et al. Factors associated with weight loss after gastric bypass. Arch Surg. 2008;143:877–883; discussion 884.
Melton GB, Steele KE, Schweitzer MA, et al. Suboptimal weight loss after gastric bypass surgery: correlation of demographics, comorbidities, and insurance status with outcomes. J Gastrointest Surg. 2008;12:250–5.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18:648–51.
Cooper TC, Simmons EB, Webb K, et al. Trends in weight regain following Roux-en-Y gastric bypass (RYGB) bariatric surgery. Obes Surg. 2015;25:1474–81.
Monaco-Ferreira DV, Leandro-Merhi VA. Weight regain 10 years after Roux-en-Y gastric bypass. Obes Surg. 2017;27:1137–44.
Swift DL, McGee JE, Earnest CP, et al. The effects of exercise and physical activity on weight loss and maintenance. Prog Cardiovasc Dis. 2018;61:206–13.
Hills AP, Street SJ, Byrne NM. Physical activity and health. Adv Food Nutr Res. 2015. p. 77–95.
Warburton DER, Bredin SSD. Health benefits of physical activity. Curr Opin Cardiol. 2017;32:541–56.
Chin S-H, Kahathuduwa CN, Binks M. Physical activity and obesity: what we know and what we need to know*. Obes Rev. 2016;17:1226–44.
King WC, Chen J-Y, Bond DS, et al. Objective assessment of changes in physical activity and sedentary behavior: pre- through 3 years post-bariatric surgery. Obesity (Silver Spring, Md.). 2015;23:1143–50.
King WC, Hsu JY, Belle SH, et al. Pre- to postoperative changes in physical activity: report from the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2). Surg Obes Relat Dis. 2012;8:522–32.
Bellicha A, Ciangura C, Roda C, et al. Changes in cardiorespiratory fitness after gastric bypass: relations with accelerometry-assessed physical activity. Obes Surg Springer New York LLC. 2019;29:2936–41.
Berglind D, Willmer M, Eriksson U, et al. Longitudinal assessment of physical activity in women undergoing Roux-en-Y gastric bypass. Obes Surg. 2015;25:119–25.
Crisp AH, Verlengia R, Ravelli MN, et al. Changes in physical activities and body composition after Roux-Y gastric bypass surgery. Obes Surg. 2018;28:1665–71.
Sellberg F, Possmark S, Willmer M, et al. Meeting physical activity recommendations is associated with health-related quality of life in women before and after Roux-en-Y gastric bypass surgery. Qual Life Res. 2019;28:1497–507.
Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative physical activity changes in bariatric surgery patients: self report vs. objective measures. Obesity (Silver Spring, Md). NIH Public Access. 2010;18:2395–7.
Berglind D, Willmer M, Tynelius P, et al. Accelerometer-measured versus self-reported physical activity levels and sedentary behavior in women before and 9 months after Roux-en-Y gastric bypass. Obes Surg. Springer New York LLC. 2016;26:1463–70.
Josbeno DA, Kalarchian M, Sparto PJ, et al. Physical activity and physical function in individuals post-bariatric surgery. Obes Surg. 2011;21:1243–9.
Markwald RR, Melanson EL, Smith MR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci U S A. 2013;110:5695–700.
Brondel L, Romer MA, Nougues PM, et al. Acute partial sleep deprivation increases food intake in healthy men. Am J Clin Nutr. 2010;91:1550–9.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring, Md.). 2008;16:643–53.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62.
Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. Int J Obes. 2008;32:1825–34.
Toor P, Kim K, Buffington CK. Sleep quality and duration before and after bariatric surgery. Obes Surg. 2012;22:890–5.
Marshall NS, Grunstein RR, Peltonen M, et al. Changes in sleep duration and changes in weight in obese patients: the Swedish Obese Subjects Study. Sleep Biol Rhythms. 2010;8:63–71.
Christensen BJ, Schmidt JB, Nielsen MS, et al. Patient profiling for success after weight loss surgery (GO Bypass study): an interdisciplinary study protocol. Contemp Clin Trials Commun. 2018;10:121–30.
Sadeh A, Sharkey M, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep. 1994;17:201–7.
Santos-Lozano A, Santín-Medeiros F, Cardon G, et al. Actigraph GT3X: validation and determination of physical activity intensity cut points. Int J Sports Med. 2013;34:975–82.
Rothney MP, Brychta RJ, Schaefer EV, et al. Body composition measured by dual-energy x-ray absorptiometry half-body scans in obese adults. Obesity. 2009;17:1281–6.
Westerterp KR, Donkers JHHLM, Fredrix EWHM, et al. Energy intake, physical activity and body weight: a simulation model. Br J Nutr. Cambridge University Press (CUP). 1995;73:337–47.
ActiGraph. What is the difference among the Energy Expenditure Algorithms? 2018. p. https://actigraphcorp.force.com/support/s/article/.
ActiGraph. Estimates from activity counts using the potential energy method. 1998. p. https://www.theactigraph.com/research-database/kca.
R. Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing version 3.3.2, Vienna, Austria 2016. URL http://www.R-project.org/.
Jacobi D, Ciangura C, Couet C, et al. Physical activity and weight loss following bariatric surgery. Obes Rev. 2011;12:366–77.
Herring LY, Stevinson C, Davies MJ, et al. Changes in physical activity behaviour and physical function after bariatric surgery: a systematic review and meta-analysis. Obes Rev Blackwell Publishing Ltd. 2016;17:250–61.
Nielsen MS, Christensen BJ, Ritz C, et al. Roux-en-Y gastric bypass and sleeve gastrectomy does not affect food preferences when assessed by an ad libitum buffet meal. Obes Surg. 2017;27:2599–605.
Chaston TB, Dixon JB, O’Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes. 2007;31:743–50.
Nielsen MS, Rasmussen S, Just Christensen B, et al. Bariatric surgery does not affect food preferences, but individual changes in food preferences may predict weight loss. Obesity. 2018;26:1879–87.
Gangwisch JE, Malaspina D, Boden-Albala B, et al. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. American Academy of Sleep Medicine. 2005;28:1289–96.
Quante M, Kaplan ER, Rueschman M, et al. Practical considerations in using accelerometers to assess physical activity, sedentary behavior, and sleep. Sleep Health. Elsevier Inc. 2015:275–84.
Acknowledgments
We wish to thank the staff at Bariatric Clinic, Køge Hospital, Denmark, the staff, and master’s students at the Department of Nutrition, Exercise and Sports, University of Copenhagen, Denmark, for helping with recruitment and data collection, and Lene Stevner for support with the protocol. A special thanks to all the participants in the GO Bypass study.
Funding
This study was carried out as part of the research program “Governing Obesity” funded by the University of Copenhagen Excellence Programme for Interdisciplinary Research (www.go.ku.dk). Additional funding was obtained from the Danish Diabetes Academy supported by the Novo Nordisk Foundation, the Lundbeck Foundation, and the Aase and Ejnar Danielsens Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in the study were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nielsen, M.S., Alsaoodi, H., Hjorth, M.F. et al. Physical Activity, Sedentary Behavior, and Sleep Before and After Bariatric Surgery and Associations with Weight Loss Outcome. OBES SURG 31, 250–259 (2021). https://doi.org/10.1007/s11695-020-04908-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04908-3