Abstract
Background
Obesity is a risk factor for postoperative pulmonary complications (PPCs). Recent studies have reported the pulmonary protective role of the kappa opioid receptor (KOR). Butorphanol is a narcotic with strong KOR agonist action, and the role in pulmonary protection is uncertain. Here, we hypothesized that butorphanol exerts protective effects on pulmonary function in patients with obesity undergoing laparoscopic bariatric surgery.
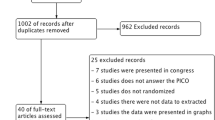
Methods
Patients with a body mass index ≥ 30 kg/m2 scheduled for laparoscopic bariatric surgery were randomized to receive butorphanol or normal saline. Butorphanol was administered as an initial loading dose of 10 μg/kg at 5 min before induction followed by 5 μg/(kg h) during surgery. The primary outcome was arterial-alveolar oxygen tension ratio (a/A ratio). Secondary outcomes included other pulmonary variables, biomarkers reflecting pulmonary injury, and incidence of PPCs within 7 days after surgery.
Results
Patients in the butorphanol group had a significantly higher a/A ratio at 1 h after the operation began (68 ± 7 vs. 55 ± 8, P < 0.001), end of the operation (73 ± 8 vs. 59 ± 7, P < 0.001), and 1 h after extubation (83 ± 9 vs. 70 ± 5, P < 0.001) compared with those in the control group. In addition, in the butorphanol group, dead space to tidal volume ratios were significantly lower than those in the control group at the same time points (all P < 0.001). In the control group, the levels of biomarkers reflecting pulmonary injury were significantly higher than those in the butorphanol group at 3 h, 6 h, 12 h, and 24 h postoperatively (P < 0.001). The incidence of PPCs was similar in both groups.
Conclusion
Butorphanol administration protected pulmonary function by improving oxygenation and reducing dead space ventilation in patients with obesity undergoing laparoscopic bariatric surgery. Butorphanol may therefore provide clinical benefits in patients with obesity.



Similar content being viewed by others
Change history
29 June 2020
In the original article some of the references were ordered incorrectly.
References
Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Ball L, Hemmes SNT, Serpa Neto A, et al. Intraoperative ventilation settings and their associations with postoperative pulmonary complications in obese patients. Br J Anaesth. 2018;121(4):899–908.
Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS - an observational study in 29 countries. Eur J Anaesthesiol. 2017;34(8):492–507.
Fernandez-Bustamante A, Frendl G, Sprung J, et al. Postoperative pulmonary complications, early mortality, and hospital stay following noncardiothoracic surgery: a multicenter study by the Perioperative Research Network Investigators. JAMA Surg. 2017;152(2):157–66.
Shashaty MG. Physiological and management implications of obesity in critical illness. Ann Am Thorac Soc. 2014;11(8):1286–97.
Tang J, Yan H. Inflammation and oxidative stress in obesity-related glomerulopathy. Int J Nephrol. 2012;2012:608397.
Reho JJ, Rahmouni K. Oxidative and inflammatory signals in obesity-associated vascular abnormalities. Clin Sci (Lond). 2017;131(14):1689–700.
Aroor AR, Jia G, Sowers JR. Cellular mechanisms underlying obesity-induced arterial stiffness. Am J Phys Regul Integr Comp Phys. 2018;314(3):R387–8.
Schinzari F, Tesauro M, Cardillo C. Endothelial and perivascular adipose tissue abnormalities in obesity-related vascular dysfunction: novel targets for treatment. J Cardiovasc Pharmacol. 2017;69(6):360–8.
Gutt CN, Müller-Stich BP. Success and complication parameters for laparoscopic surgery: a benchmark for natural orifice transluminal endoscopic surgery. Endoscopy. 2009;41(01):36–41.
Nishiyama T, Kohno Y. Anesthesia for bariatric surgery. Obes Surg. 2012;22(2):213–9.
Rivas E, Arismendi E, Agustí A, et al. Ventilation/perfusion distribution abnormalities in morbidly obese subjects before and after bariatric surgery. Chest. 2015;147(4):1127–34.
Tai KK, Jin WQ, Chan TK. Characterization of [3H]U69593 binding sites in the rat heart by receptor binding assays. J Mol Cell Cardiol. 1991;23(11):1297–302.
Wittert G, Hope P. Tissue distribution of opioid receptor gene expression in the rat. Biochem Biophys Res Commun. 1996;218(3):877–81.
Li J, Shi QX, Fan R, et al. Vasculoprotective effect of U50,488H in rats exposed to chronic hypoxia: role of Akt-stimulated NO production. J Appl Physiol. 2013;114(2):238–44.
Li J. Role of κ-opioid receptor activation in anti-hypoxic pulmonary hypertension and its underlying mechanisms [dissertation]. China: FourthMilitary Medical University; 2017.
Wu Q, Wang HY, Li J, et al. κ-opioid receptor stimulation improves endothelial function in hypoxic pulmonary hypertension. PLoS One. 2013;8:e60850.
Cui Y, Feng N, Gu X, et al. κ-Opioid receptor stimulation reduces palmitate-induced apoptosis via Akt/eNOS signaling pathway. Lipids Health Dis. 2019;18(1):52.
Jose DE, Ganapathi P, Anish Sharma NG, et al. Postoperative pain relief with epidural buprenorphine versus epidural butorphanol in laparoscopic hysterectomies: a comparative study. Anesth Essays Res. 2016;10(1):82–7.
Wu Y, Wan J, Zhen WZ, et al. The effect of butorphanol postconditioning on myocardial ischaemia reperfusion injury in rats. Interact Cardiovasc Thorac Surg. 2014;18(3):308–12.
Huang LH, Li J, Gu JP, et al. Butorphanol attenuates myocardial ischemia reperfusion injury through inhibiting mitochondria-mediated apoptosis in mice. Eur Rev Med Pharmacol Sci. 2018;22:1819–24.
Yang L, Sun DF, Wu Y, et al. Intranasal administration of butorphanol benefits old patients undergoing H-uvulopalatopharyngoplasty: a randomized trial. BMC Anesthesiol. 2015;15(1):20.
La Colla L, Albertin A, La Colla G, et al. Predictive performance of the ‘Minto’ remifentanil pharmacokinetic parameter set in morbidly obese patients ensuing from a new method for calculating lean body mass. Clin Pharm. 2010;49(2):131–9.
The ARDS Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342(18):1301–8.
Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–50.
Mazo V, Sabaté S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121(12):219–31.
Scholes RL, Browning L, Sztendur EM, et al. Duration of anaesthesia, type of surgery, respiratory co-morbidity, predicted VO2max and smoking predict postoperative pulmonary complications after upper abdominal surgery: an observational study. Aust J Physiother. 2009;55(3):191–8.
Haines KJ, Skinner EH, Berney S, et al. Association of postoperative pulmonary complications with delayed mobilisation following major abdominal surgery: an observational cohort study. Physiotherapy. 2013;99(2):119–25.
Browning L, Denehy L, Scholes RL. The quantity of early upright mobilisation performed following upper abdominal surgery is low: an observational study. Aust J Physiother. 2007;53(1):47–52.
Parry S, Denehy L, Berney S, et al. Clinical application of the Melbourne risk prediction tool in a high-risk upper abdominal surgical population: an observational cohort study. Physiotherapy. 2014;100:47–53.
Samnani SS, Umer MF, Mehdi SH, et al. Impact of preoperative counselling on early postoperative mobilization and its role in smooth recovery. Int Sch Res Notices. 2014;2014:250536.
Boden I, Browning L, Skinner EH, et al. The LIPPSMAck POP (Lung Infection Prevention Post Surgery-Major Abdominal-with PreOperative Physiotherapy) trial: study protocol for a multi-centre randomised controlled trial. Trials. 2015;16(1):1–15.
Boden I, Skinner EH, Browning L, et al. Preoperative physiotherapy for the prevention of respiratory complications after upper abdominal surgery: pragmatic, double blinded, multicentre randomised controlled trial. BMJ. 2018;360:461–7.
Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the Observer’s Assessment of Alertness/Sedation Scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10(4):244e51.
Flier S. How to inform a morbidly obese patient on the specific risk to develop postoperative pulmonary complications using evidence-based methodology. Eur J Anaesthesiol. 2006;23(2):154–9.
Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low PEEP on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA. 2019;321(23):2292–305.
Matthay MA, Bhattacharya S, Gaver D, et al. Ventilator-induced lung injury: in vivo and in vitro mechanisms. Am J Phys Lung Cell Mol Phys. 2002;283(4):L678–82.
Zhang S, Zhou Y, Zhao L, et al. κ-Opioid receptor activation protects against myocardial ischemia-reperfusion injury via AMPK/Akt/eNOS signaling activation. Eur J Pharmacol. 2018;833:100–8.
Zhou Y, Wang Y, Wang X, et al. The protective effects of κ-opioid receptor stimulation in hypoxic pulmonary hypertension involve inhibition of autophagy through the AMPK-MTOR pathway. Cell Physiol Biochem. 2017;44(5):1965–79.
Franklin C, Fortepiani L, Nguyen T, et al. Renal responses produced by microinjection of the kappa opioid receptor agonist, U50-488H, into sites within the rat lamina terminalis. Pharmacol Res Perspect. 2015;3(2):e00117.
Peng P, Huang LY, Li J, et al. Distribution of kappa-opioid receptor in the pulmonary artery and its changes during hypoxia. Anat Rec (Hoboken). 2009;292(7):1062–7.
Shekar K, Fraser JF. Ventilator-induced lung injury. N Engl J Med. 2014;370(4):979.
Gao TT, Jiang L. Obesity exacerbates pulmonary vascular endothelial injury caused by mechanical ventilation. Int J Anesth Resu. 2018;(3):250–3. Chinese
Shah RJ, Wickersham N, Lederer DJ, et al. Preoperative plasma club (Clara) cell secretory protein levels are associated with primary graft dysfunction after lung transplantation. Am J Transplant. 2014;14(2):446–52.
Ide S, Minami M, Ishihara K, et al. Abolished thermal and mechanical antinociception but retained visceral chemical antinociception induced by butorphanol in mu-opioid receptor knockout mice. Neuropharmacology. 2008;54(8):1182–8.
Black D. The kappa opioid receptor is associated with the perception of visceral pain. Gut. 1998;43(3):312–3.
Boom M, Niesters M, Sarton E, et al. Non-analgesic effects of opioids: opioid-induced respiratory depression. Curr Pharm Des. 2012;18(37):5994–6004.
Pasternak GW. Mu opioid pharmacology: 40 years to the promised land. Adv Pharmacol. 2018;82:261–91.
Commiskey S, Fan LW, Ho IK. Butorphanol: effects of a prototypical agonist-antagonist analgesic on kappa-opioid receptors. J Pharmacol Sci. 2005;98(2):109–16.
Hardman JG, Aitkenhead AR. Estimating alveolar dead space from the arterial to end-tidal CO2 gradient: a modeling analysis. Anesth Analg. 2003;97(6):1846–51.
Acknowledgments
The authors thank Long Wang at University of Xuzhou Medical University for his stimulating discussion and help on enzyme-linked immunosorbent assay techniques.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC-81371242, NSFC-81671084); Qing Lan Project of Jiangsu province, Nature Science Foundation of Jiangsu province (BK20161175); “Six One” Project of Jiangsu province (LGY2016039); and The Science Funds for Health and Family Planning Commission of Sichuan Province (18PJ157).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the local institutional review board (XYFY2019-KL082-01).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, Xl., Zeng, S., Li, Xx. et al. The Protective Effects of Butorphanol on Pulmonary Function of Patients with Obesity Undergoing Laparoscopic Bariatric Surgery: a Double-Blind Randomized Controlled Trial. OBES SURG 30, 3919–3929 (2020). https://doi.org/10.1007/s11695-020-04755-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04755-2