Abstract
Purpose
Although the post-bariatric clinical and physical changes are well-known, the psychosocial changes in patients’ everyday life are less clear. Therefore, we tried to summarize comprehensively the currently available literature on the psychosocial changes of bariatric surgery (BS) by means of a scoping review.
Materials and Methods
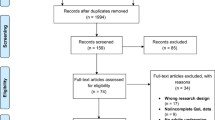
The scoping review was conducted following the Arksey and O’Malley framework, the Joanna Briggs Institute Reviewer’s Manual 2015, and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) checklist. PubMed, EMBASE, and PsycINFO were searched for data dating from January 2008 through October 2019. Only gastric bypass and sleeve gastrectomy procedures were considered for this review. To explore and describe the essence of the experienced changes deeply, only qualitative studies were included. The synthesis was performed using the qualitative content analysis technique.
Results
The literature search yielded 1420 unique records, and 1371 articles were eliminated on the basis of irrelevant title and/or abstract. Forty-nine full-text articles were reviewed. Ultimately, eight articles were included in this scoping review. The qualitative content analysis emerged in 12 categories, which were further condensed into three major thematic areas, namely, “subjective self-image,” “interpersonal relationships,” and “it’s not all gold that glitters,” which reflect the post-operative psychosocial changes.
Conclusion
A wide range of psychosocial changes occurs following bariatric surgery. To maintain the improvements and to prevent negative changes, long-term support by specially trained health professionals is crucial.


Similar content being viewed by others
References
WHO, Obesity: preventing and managing the global epidemic. Report of a WHO consultation. WHO Technical Report Series 894, Geneva 2000.
CColquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014; 8(CD003641). https://doi.org/10.1002/14651858.CD003641.pub4.
American Society for Metabolic and Bariatric Surgery: bariatric surgery misconceptions. Available from: https://asmbs.org/patients/bariatric-surgery-misconceptions. Accessed 29 Aug 2019.
Coulman KD, Abdelrahman T, Owen-Smith A, et al. Patient-reported outcomes in bariatric surgery: a systematic review of standards of reporting. Obes Rev. 2013;14(9):707–20.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23(4):427–36.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial–a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273(3):219–34.
Thonney B, Pataky Z, Badel S, et al. The relationship between weight loss and psychosocial functioning among bariatric surgery patients. Am J Surg. 2010;199(2):183–8.
Chang S-H, Stoll CRT, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Peters M, et al. The Joanna Briggs Institute Reviewers’ Manual 2015: methodology for JBI scoping reviews. 2015.
Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation The PRISMA-ScR statement. Ann Intern Med. 2018;169(7):467–73.
Estimate of Bariatric Surgery Numbers, 2011–2017. Available from: https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers. Accessed 17 May 2019.
Spaniolas K, Kasten KR, Brinkley J, et al. The changing bariatric surgery landscape in the USA. Obes Surg. 2015;25(8):1544–6.
Courcoulas AP, Christian NJ, Belle SH, et al. Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity weight and health 3 years after bariatric surgery weight and health 3 years after bariatric surgery. JAMA. 2013;310(22):2416–25.
Silva LB, Oliveira BMPM, Correia F. Evolution of body composition of obese patients undergoing bariatric surgery. Clinical Nutrition ESPEN, 2019
Erlingsson C, Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7(3):93–9.
Mayring P. Qualitative Inhaltsanalyse. in Mey G, Mruck K. (eds) Handbuch Qualitative Forschung in der Psychologie. VS Verlag für Sozialwissenschaften; 2010. pp.601–613. https://doi.org/10.1007/978-3-531-92052-8_42.
Mariano ML, de Paula MA, Bassi DG, et al. Bariatric surgery: impact on sexuality of the obese person. Rev Col Bras Cir. 2014;41(6):412–20.
Mariano ML, Monteiro CS, de Paula MA. Bariatric surgery: its effects for obese in the workplace. Rev Gaucha Enferm. 2013;34(3):38–45.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269.
Jensen JF, Petersen MH, Larsen TB, et al. Young adult women’s experiences of body image after bariatric surgery: a descriptive phenomenological study. J Adv Nurs. 2014;70(5):1138–49.
Groven KS, Råheim M, Engelsrud G. “My quality of life is worse compared to my earlier life” living with chronic problems after weight loss surgery. Int J Qual Stud Health Well Being. 2010;5(4):1–15.
Faccio E, Nardin A, Cipolletta S. Becoming ex-obese: narrations about identity changes before and after the experience of the bariatric surgery. J Clin Nurs. 2016;25(11–12):1713–20.
Geraci AA, Brunt AR, Marihart CL. A qualitative analysis of female bariatric patients after the first two years postoperative. Bariatr Surg Pract Patient Care. 2014;9(2):66–71.
Heidmann J, Grønkjær M. Health-related quality of life six years after gastric bypass: a mixed methods study. J Clin Nurs. 2015;10(2):56–61.
Lier HO, Aastrom S, Rortveit K. Patients’ daily life experiences five years after gastric bypass surgery--a qualitative study. J Clin Nurs. 2016;25(3–4):322–31.
Perdue TO, Schreier A,Neil J, Carels R. and Swanson M. A concept analysis of disturbed body image in bariatric surgery patients. Int J Nurs Terminol Knowledge. 2020;31:74-81. https://doi.org/10.1111/2047-3095.12220.
Warholm C, Øien AM, Råheim M. The ambivalence of losing weight after bariatric surgery. Int J Qual Stud Health Well Being. 2014;9(1):22876.
Coulman KD, MacKichan F, Blazeby JM, et al. Patient experiences of outcomes of bariatric surgery: a systematic review and qualitative synthesis. Obes Rev. 2017;18(5):547–59.
Sarwer DB, Dilks RJ, West-Smith L. Dietary intake and eating behavior after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis. 2011;7(5):644–51.
Beltrán-Carrillo VJ, Jiménez-Loaisa A, Jennings G, et al. Exploring the socio-ecological factors behind the (in) active lifestyles of Spanish post-bariatric surgery patients. Int J Qual Stud Health Well Being. 2019;14(1):1626180.
Conceição E, Teixeira F, Rodrigues T, et al. Problematic eating behaviors after bariatric surgery: a national study with a Portuguese sample. Acta Medica Port. 2018;31(11):633–40.
Benson-Davies S, Davies ML, Kattelmann K. Understanding eating and exercise behaviors in post Roux-en-Y gastric bypass patients: a quantitative and qualitative study. Diabetes Metab Syndr Obes.. 2013;8(2):61–8.
McGrice M, Don Paul K. Interventions to improve long-term weight loss in patients following bariatric surgery: challenges and solutions. Diabetes Metab Syndr Obes. 2015;8:263–74.
Castaneda D, Popov VB, Wander P, et al. Risk of suicide and self-harm is increased after bariatric surgery—a systematic review and meta-analysis. Obes Surg. 2019;29(1):322–33.
Müller A, Hase C, Pommnitz M, et al. Depression and suicide after bariatric surgery. Curr Psychiatry Rep. 2019;21(9):84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
For this type of study, formal consent is not required.
Informed Consent
Informed consent does not apply.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Additional File 1:
Search Strategy for PubMed, PsycINFO, and Embase (DOCX 20 kb).
Additional File 2:
Excluded publications (DOCX 25 kb).
Additional File 3:
Synthesis of results and illustrative quotes (DOCX 21 kb).
Rights and permissions
About this article
Cite this article
Doni, K., Breuing, J. & Pieper, D. Psychosocial Changes of Bariatric Surgery in Patients’ Everyday Life: a Scoping Review. OBES SURG 30, 2949–2956 (2020). https://doi.org/10.1007/s11695-020-04621-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04621-1