Abstract
Purpose
Obesity is a disease of increasing prevalence. There is minimal research on the safety of sedation for general endoscopic procedures among super obese patients (BMI ≥ 50). The aim of our study was to evaluate the safety of moderate sedation and endoscopic procedural outcomes for super obese patients in a case-control study.
Materials and Methods
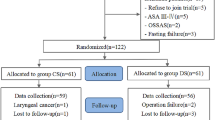
We completed an age and sex–matched case-control study comparing 132 super obese patients with 132 non-obese controls. We assessed intra-procedure adverse events, delayed adverse events, doses of sedation medication used, and procedure duration at a tertiary care setting.
Results
The mean BMI for the obese cohort was 55.6 compared with 22.5 for the controls (P < 0.001). The mean intra-procedure fentanyl and midazolam dose was higher for the obese patients compared with the controls, fentanyl 180 mcg, midazolam 7.7 mg vs fentanyl 148 mcg, midazolam 6.4 mg, respectively (P < 0.001). There was a significantly higher percentage of brief intra-procedure hypoxia (oxygen blood saturation < 90%) for the obese patients compared with the controls, 5% vs 0% (P = 0.02). There was no difference in delayed adverse events with 2% of the cases and 2% of the controls having delayed adverse events (P = 1.0). Procedure completion rates were 100% for both cases and controls.
Conclusion
General endoscopic procedures can be safely and effectively performed in super obese patients with moderate sedation. Brief intra-procedure hypoxia more commonly occurs in super obese patients, and higher medication doses are required.
Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315:2284–91.
Ogden CL, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS data brief, no 219. Hyattsville, MD: National Center for Health Statistics. 2015.
Sturm R. Increases in clinically severe obesity in the United States, 1986-2000. Arch Intern Med. 2003;163(18):2146–8.
Hensrud DD, Klein S. Extreme obesity: a new medical crisis in the United States. Mayo Clin Proc. 2006;81(10 Suppl):S5–10.
Cheryl D. Fryar, Margaret D. Carroll and Cynthia L. Ogden Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2015–2016. www.cdc.gov
Joseph DA, Meester RG, Zauber AG, et al. Colorectal cancer screening: estimated future colonoscopy need and current volume and capacity. Cancer. 2016;122(16):2479–86.
Mcquaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc. 2008;67(6):910–23.
Cohen LB, Wecsler JS, Gaetano JN, et al. Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol. 2006;101(5):967–74.
Lichtenstein DR, Jagannath S, Baron TH, et al. Clinical guideline on sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68(5):815–26.
Sharma VK, Nguyen CC, Crowell MD, et al. Cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66:27–34.
Early DS, Lightdale JR, Vargo JJ, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018;87(2):327–37.
Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96:1004–17.
World Health Organization: Obesity and overweight. http://www.who.int/mediacentre/factsheets. Accessed 12/2018.
Passannante AN, Rock P. Anesthetic management of patients with obesity and sleep apnea. Anesthesiol Clin North Am. 2005;23:479–91.
Shibutani K, Inchiosa MA, Sawada K, et al. Accuracy of pharmacokinetic models for predicting plasma fentanyl concentrations in lean and obese surgical patients: derivation of dosing weight (‘pharmacokinetic mass’). Anesthesiology. 2004;101:603–13.
van Rongen A, Vaughns JD, Moorthy GS, et al. Population pharmacokinetics of midazolam and its metabolites in overweight and obese adolescents den Anker. Br J Clin Pharmacol. 2015 Nov;80(5):1185–96.
Shibutani K, Inchiosa Jr MA, Sawada K, et al. Pharmacokinetic mass of fentanyl for postoperative analgesia in lean and obese patients. Br J Anaesth. 2005 Sep;95(3):377–83.
Carey WD. Indications, contraindications and complications of upper gastrointestinal endoscopy. Gastroenterologic Endoscopy. Philadelphia:WB Saunders;1987. pp 296–306.
Rankin GB. Indications, contraindications and complications of colonoscopy. Gastroenterologic Endoscopy. Philadelphia:WB Saunders;1987. pp 868–880.
Vargo JJ, Niklewski PJ, Williams JL, et al. Patient safety during sedation by anesthesia professionals during routine upper endoscopy and colonoscopy: an analysis of 1.38 million procedures. Gastrointest Endosc. 2017;85(1):101–8.
Waring JP, Baron TH, Hirota WK, et al. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. Gastrointest Endosc. 2003;58(3):317–22.
Freeman ML. Sedation and monitoring for gastrointestinal endoscopy. Gastrointest Endosc Clin N Am. 1994;4:475–99.
Dhariwal A, Plevris JN, Lo NT, et al. Age, anemia, and obesity-associated oxygen desaturation during upper gastrointestinal endoscopy. Gastrointest Endosc. 1992;38(6):684–8.
Khan I, Chatterjee AB, Bellinger CR, et al. Sedation for bronchoscopy and complications in obese patients. Respiration. 2016;92(3):158–65.
Madan AK, Tichansky DS, Isom J, et al. Monitored anesthesia care with propofol versus surgeon-monitored sedation with benzodiazepines and narcotics for preoperative endoscopy in the morbidly obese. Obes Surg. 2008;18:545–8.
Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013;173(7):551–6.
Bielawski B, Hookey LC, Sutradhar R, et al. Anesthesia assistance in outpatient colonoscopy and risk of aspiration pneumonia, bowel perforation, and splenic injury. Gastroenterology. 2018;154(1):77–85.
Faigel DO, Baron TH, Goldstein JL, et al. Guidelines for the use of deep sedation and general anesthesia for GI endoscopy. Gastrointest Endosc. 2002;56:613–7.
Jirapinyo P, Abu Dayyeh BK, Thompson CC. Conscious sedation for upper endoscopy in the gastric bypass patient: prevalence of cardiopulmonary adverse events and predictors of sedation requirement. Dig Dis Sci. 2014;59(9):2173–7.
Matharoo M, Thomas-Gibson S, Haycock A, et al. Implementation of an endoscopy safety checklist. Frontline Gastroenterol. 2014 Oct;5(4):260–5.
Matharoo M, Haycock A, Sevdalis N, et al. A prospective study of patient safety incidents in gastrointestinal endoscopy. Endosc Int Open. 2017 Jan;5(1):E83–9.
Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2006 Apr;63(4 Suppl):S16–28.
Cohen J, Safdi MA, Deal SE, et al. Quality indicators for esophagogastroduodenoscopy. Gastrointest Endosc. 2006 Apr;63(4 Suppl):S10–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Benson, M., Hubers, J., Caldis, M. et al. Safety and Efficacy of Moderate Sedation in Super Obese Patients Undergoing Lower and Upper GI Endoscopy: a Case-Control Study. OBES SURG 30, 3466–3471 (2020). https://doi.org/10.1007/s11695-020-04600-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04600-6