Abstract
Rationale
The length of hospital stay after bariatric surgery has decreased rapidly in recent years to an average of 1 day (one midnight). The transition from a controlled hospital environment to home environment may be a big step for patients. For these patients, home monitoring can be a substitute.
Methods
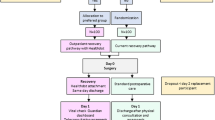
A pilot study of 84 morbidly obese patients undergoing either laparoscopic Roux-Y gastric bypass (LRYGB) or laparoscopic sleeve gastrectomy (LGS) was performed. Home monitoring consisted of daily contact via video consultation and measurement of vital signs at home. The primary outcome was feasibility of home monitoring. Secondary outcomes were complications and patient satisfaction measured with a questionnaire (PSQ-18).
Results
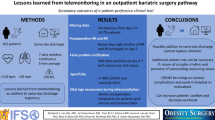
In 77 of the 84 patients (92%), videoconference was possible on day 1, 74 patients (88%) on day 2 and 76 patients (90%) on day 3. Four patients (5%) were never reached. On day 1, 52 patients (62%) performed all instructed measurements, on day 2, 49 patients (58%) and on day 3, 63 patients (75%). Only 47 out of 84 patients (56%) measured the instructed amount of times on all 3 days. High satisfaction rates were reported in the patients receiving home monitoring.
Conclusion
Our first experience with home monitoring was disappointing since home monitoring of vital signs had poor compliance and not all patients were able to use the application. Further refinement of the home monitoring tool is needed to increase compliance and utility of the tool.

Similar content being viewed by others
References
WHO | Obesity and overweight. Available from: http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
DATO Jaarrapportage. 2017
Kim DD, Basu A. Estimating the medical care costs of obesity in the United States: systematic review, meta-analysis, and empirical analysis. Value Health. 2016;19(5):602–13.
Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011;12(2):131–41.
Effertz T, Engel S, Verheyen F, et al. The costs and consequences of obesity in Germany: a new approach from a prevalence and life-cycle perspective. Eur J Health Econ. 2016;17(9):1141–58.
Blanchet MC, Gignoux B, Matussiere Y, et al. Experience with an enhanced recovery after surgery (ERAS) program for bariatric surgery: comparison of MGB and LSG in 374 patients. Obes Surg. 2017;27(7):1896–900.
Acquafresca PA, Palermo M, Rogula T, et al. Early surgical complications after gastric by-pass: a literature review. Arq Bras Cir Dig. 2015;28(1):74–80.
Fried M, Yumuk V, Oppert JM, et al. Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg. 2014;24(1):42–55.
Clinicards Available from: https://www.synappz.nl
Weenk M, van Goor H, van Acht M, et al. A smart all-in-one device to measure vital signs in admitted patients. PLoS One. 2018;13(2):e0190138.
Marshall GN HR. RAND Corporation; The patient satisfaction questionnaire short form (PSQ-18). 1994 (Santa Monica, CA):P. 7865.
Morrow E, Bruce DM, Bruce E, et al. Post surgical review of bariatric surgery patients: a feasibility study of multidisciplinary follow up using videoconferencing. Clin Pract Epidemiol Ment Health. 2011;7:84–8.
Sudan R, Salter M, Lynch T, et al. Bariatric surgery using a network and teleconferencing to serve remote patients in the veterans administration health care system: feasibility and results. Am J Surg. 2011;202(1):71–6.
Vilallonga R, Lecube A, Fort JM, et al. Internet of things and bariatric surgery follow-up: comparative study of standard and IoT follow-up. Minim Invasive Ther Allied Technol. 2013;22(5):304–11.
Bradley LE, Forman EM, Kerrigan SG, et al. Project HELP: a remotely delivered behavioral intervention for weight regain after bariatric surgery. Obes Surg. 2017;27(3):586–98.
Bradley LE, Forman EM, Kerrigan SG, et al. A pilot study of an acceptance-based behavioral intervention for weight regain after bariatric surgery. Obes Surg. 2016;26(10):2433–41.
Zhang MW, Ho RC, Hawa R, et al. Pilot implementation and user preferences of a bariatric after-care application. Technol Health Care. 2015;23(6):729–36.
Bragg DD, Edis H, Clark S, et al. Development of a telehealth monitoring service after colorectal surgery: a feasibility study. World J Gastrointest Surg. 2017;9(9):193–9.
Bradley LE, Thomas JG, Hood MM, et al. Remote assessments and behavioral interventions in post-bariatric surgery patients. Surg Obes Relat Dis. 2018;
Coldebella B, Armfield NR, Bambling M, et al. The use of telemedicine for delivering healthcare to bariatric surgery patients: a literature review. J Telemed Telecare. 2018;24(10):651–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nijland, L.M.G., van Veen, R.N., Ruys, A.T. et al. Feasibility of Postoperative Home Monitoring Using Video Consultation and Vital Sign Monitoring of Bariatric Patients. OBES SURG 30, 2369–2374 (2020). https://doi.org/10.1007/s11695-020-04500-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04500-9