Abstract
Background and Objectives
Surgical trauma, pain and opioids can cause nausea, vomiting, ileus and increased length of hospital stay. The primary objective of the study was to evaluate the time to recovery of gastrointestinal function and the time to meet hospital discharge criteria after laparoscopic bariatric surgery with intraoperative intravenous lidocaine administration. Secondary objectives were to evaluate morphine consumption during the first 24 h and the side effects of opioids.
Methods
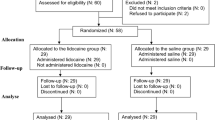
Fifty-eight patients aged 18 to 60 years who underwent bariatric surgery were allocated into two groups. Group 1 patients received intravenous lidocaine (1.5 mg/kg) 5 min before induction of anaesthesia, followed by infusion (2 mg/kg/h) until the end of surgery. Group 2 patients were given 0.9% saline solution (placebo) and infusion of 0.9% saline solution during surgery, in same volume as group 1. Anaesthesia was performed with fentanyl (5 μg/kg), propofol (2 mg/kg), rocuronium (0.6 mg/kg) and sevoflurane. Postoperative patient-controlled analgesia was with morphine. There were two groups that were evaluated: time to recovery of gastrointestinal function and time to meet discharge criteria.
Results
There was no significant difference between groups regarding the time to first flatus, time to meet discharge criteria and occurrence of side effects. Consumption of intraoperative sevoflurane and morphine over 24 h was significantly lower in the lidocaine group. Side effects observed were nausea and vomiting, with no difference between groups.
Conclusions
Perioperative intravenous lidocaine is feasible and easily accessible when administered at appropriate doses. Lidocaine reduces morphine consumption.

Similar content being viewed by others
References
Berbiglia L, Zografakis JG, Dan AG. Laparoscopic Roux-en-Y gastric bypass: surgical technique and perioperative care. Surg Clin N Am. 2016;96:773–94.
Xu LL, Zhou XQ, Yi PS, et al. Alvimopan combined with enhanced recovery strategy for managing postoperative ileus after open abdominal surgery: a systematic review and meta-analysis. J Surg Res. 2016;203:211–21.
Mannaerts GHH, Van Mil SR, Stepaniak PS, et al. Results of implementing an enhanced recovery after bariatric surgery (ERABS) protocol. Obes Surg. 2016;26(2):303–12.
Marret E, Rolin M, Beaussier M, et al. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008;95:1331–8.
Mortensen K, Nilsson M, Slim K, et al. Consensus guidelines for enhanced recovery after gastrectomy. BJS. 2014;101:1209–29.
Kim TH, Kang H, Choi YS, et al. Pre- and intraoperative lidocaine injection for preemptive analgesics in laparoscopic gastrectomy: a prospective, randomized, double-blind, placebo-controlled study. J Palarpendosc Advanced Surg Tech. 2013;23(8):663–8.
Terkawi AS, Tsang S, Kazemi A, et al. A clinical comparison of intravenous and epidural local anesthetic for major abdominal surgery. Reg Anesth Pain Med. 2016;41:28–36.
Carter J, Elliott S, Kaplan J, et al. Predictors of hospital stay following laparoscopic gastric bypass: analysis of 9,593 patients from the National Surgical Quality Improvement Program. Surg Obes Relat Dis. 2015;11(2):288–94.
Han PY, Duffull SB, Kirkpatrick CM, et al. Dosing in obesity: a simple solution to a big problem. Clin Pharmacol Ther. 2007;82:505–8.
Benumof JL. Obstructive sleep apnea in the adult obese patient: implications for airway management. J Clin Anesth. 2001;13:144–56.
Pang KP. Identifying patients who need close monitoring during and after upper airway surgery for obstructive sleep apnoea. J Laryngol Otol. 2006;120:655–60.
Chung SA, Yuan H, Chung F. A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008;107:1543–63.
Dallal RM, Trang A. Analysis of perioperative outcomes, length of hospital stay and readmission rate after gastric bypass. Surg Endosc. 2012;26(3):754–8.
Reyes-Pérez A, Sánchez-Aguilar H, Velázquez-Fernández D, et al. Analysis of causes and risk factors for hospital readmission after Roux-en-Y gastric bypass. Obes Surg. 2016;26(2):257–60.
Barreca M, Renzi C, Tankel J, et al. Is there a role for enhanced recovery after laparoscopic bariatric surgery? Preliminary results from a specialist obesity treatment center. Surg Obes Rel Dis. 2016;12:119–26.
Oliveira Jr GS, Duncan K, Fitzgerald P, et al. Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: a randomized double-blinded placebo-controlled trial. Obes Surg. 2014;24:212–8.
De Oliveira CM, Issy AM, Sakata RK. Intraoperative intravenous lidocaine. Rev Bras Anestesiol. 2010;60:325–33.
Vigneault L, Turgeon AF, Côté D, et al. Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth. 2011;58(1):22–37.
Kranke P, Jokinem J, Pace NL, et al. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery (review). Cochrane Database Syst Rev. 2015:CD009642. https://doi.org/10.1002/14651858
Weibel S, Jokinem J, Pace NL, et al. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016;116:770–80.
Estebe JP. Intravenous lidocaine. Best Practice Res Clin Anaesthesiol. 2017;31:513–21.
Khorgami Z, Petrosky JA, Andalib A, et al. Fast track bariatric surgery: safety of discharge on the first postoperarative day after bariatric surgery. Surg Obes Relat Dis. 2017;13:273–80.
Dunn LK, Durieux ME. Perioperative use of intravenous lidocaine. Anesthesiology. 2017 Apr;126(4):729–37. https://doi.org/10.1097/ALN.0000000000001527.
Ventham NT, Kennedy ED, Brady RR, et al. Efficacy of intravenous lidocaine for postoperative analgesia following laparoscopic surgery: a meta-analysis. World J Surg. 2015;39:2220–34.
Deneuvy A, Slim K, Sodji M, et al. Implementation of enhanced recovery programs for bariatric surgery. Results from the francophone large-scale database. Surg Obes Relat Dis. 2018;14:99–105.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sakata, R.K., de Lima, R.C., Valadão, J.A. et al. Randomized, Double-Blind Study of the Effect of Intraoperative Intravenous Lidocaine on the Opioid Consumption and Criteria for Hospital Discharge After Bariatric Surgery. OBES SURG 30, 1189–1193 (2020). https://doi.org/10.1007/s11695-019-04340-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04340-2