Abstract
Introduction
Sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) are common bariatric surgeries that can alter physiological barriers against gastroesophageal reflux disease (GERD). We investigated the prevalence and potential physiologic underpinnings of erosive esophagitis (EE) after bariatric surgery in a large cohort with long-term follow-up.
Methods
This is a retrospective analysis of 517 patients who underwent an esophagogastroduodenoscopy after SG or RYGB. A matched case-control sub-study was conducted to compare physiologic contributors of GERD after SG with a pre-operative cohort using high-resolution manometry.
Results
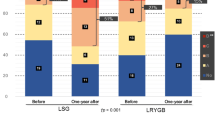
Consecutive post-SG and post-RYGB patients (body mass index (BMI) 34 ± 9.1 kg/m2, age 49 ± 12.4 years, 83% female) were included. EE was more prevalent after SG than RYGB (37.9% vs. 17.6%, p = 0.0001), including severe EE (10.7% vs. 3.1%, p = 0.0007). Post-SG EE remained more prevalent after adjusting for multiple confounders (OR = 2.47, p = 0.0012). In a matched case-control analysis, prevalence of EE was 31% in 39 SG patients compared with 13% in 40 pre-bariatric surgery patients with GERD and obesity (p = 0.044). Significant physiologic changes conducive to GERD was observed after SG including (1) decrease resting lower esophageal sphincter (LES) (mmHg) pressure (21.3 ± 14.1 vs. 39.8 ± 35.6, p = 0.004), and (2) lower maximal distal contractile integral (DCI) (mmHg-s-cm) (3814.8 ± 2684.8 vs. 5111.8 ± 7713, p = 0.034).
Conclusion
EE is more prevalent after SG compared with RYGB in a pre-bariatric surgery cohort with GERD. SG is associated with significant esophageal physiologic changes conducive to GERD and its clinical consequences.



Similar content being viewed by others
References
Ozanan M. Laparoscopic sleeve gastrectomy. J Med Insight. 2017;
Kayaalp C, Sümer F, Abdullayev A. Laparoscopic Roux-en-Y gastric bypass. Laparosc Endosc Surg Sci. 2016;23(4):110–8.
Sheppard CE, Sadowski DC, de Gara CJ, et al. Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity. Obes Surg. 2015;25(5):763–8.
Kindel TL, Oleynikov D. The improvement of gastroesophageal reflux disease and Barrett's after bariatric surgery. Obes Surg. 2016;26(4):718–20.
Barr AC, Frelich MJ, Bosler ME, et al. GERD and acid reduction medication use following gastric bypass and sleeve gastrectomy. Surg Endosc. 2017;31(1):410–5.
Laffin M et al. Sleeve gastrectomy and gastroesophageal reflux disease. J Obes. 2013;2013:741097–7.
Carabotti M, Avallone M, Cereatti F, et al. Usefulness of upper gastrointestinal symptoms as a driver to prescribe gastroscopy in obese patients candidate to bariatric surgery. A prospective study. Obes Surg. 2016;26(5):1075–80.
Soricelli E, Casella G, Baglio G, et al. Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy. Surg Obes Relat Dis. 2018;14(6):751–6.
Lim CH, Lee PC, Lim E, et al. Correlation between symptomatic gastro-esophageal reflux disease (GERD) and erosive esophagitis (EE) post-vertical sleeve gastrectomy (VSG). Obes Surg. 2019;29(1):207–14.
Santo MA et al. Endoscopic changes related to gastroesophageal reflux disease: comparative study among bariatric surgery patients. Arq Bras Cir Dig. 2015;28(Suppl 1):36–8.
Estevez-Fernandez S et al. Esophagogastric pathology in morbid obese patient: preoperative diagnosis, influence in the selection of surgical technique. Rev Esp Enferm Dig. 2015;107(7):408–12.
Tai CM, Huang CK, Lee YC, et al. Increase in gastroesophageal reflux disease symptoms and erosive esophagitis 1 year after laparoscopic sleeve gastrectomy among obese adults. Surg Endosc. 2013;27(4):1260–6.
Czeczko LE et al. Correlation between pre and postoperative upper digestive endoscopy in patients who underwent roux-en-y gastrojejunal bypass. Arq Bras Cir Dig. 2016;29(1):33–7.
Miguel GP et al. Erosive esophagitis after bariatric surgery: banded vertical gastrectomy versus banded Roux-en-Y gastric bypass. Obes Surg. 2011;21(2):167–72.
Braghetto I, Korn O, Csendes A, et al. Laparoscopic treatment of obese patients with gastroesophageal reflux disease and Barrett’s esophagus: a prospective study. Obes Surg. 2012;22(5):764–72.
Csendes JA et al. Effects of gastric bypass on erosive esophagitis in obese subjects. Rev Med Chil. 2006;134(3):285–90.
Braghetto I, Lanzarini E, Korn O, et al. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes Surg. 2010;20(3):357–62.
El-Hadi M et al. The effect of bariatric surgery on gastroesophageal reflux disease. Can J Surg. 2014;57(2):139–44.
Del Genio G et al. Sleeve gastrectomy and development of “de novo” gastroesophageal reflux. Obes Surg. 2014;24(1):71–7.
Xu XR, Li ZS, Zou DW, et al. Role of duodenogastroesophageal reflux in the pathogenesis of esophageal mucosal injury and gastroesophageal reflux symptoms. Can J Gastroenterol. 2006;20(2):91–4.
Li MJ, Li Q, Sun M, et al. Comparative effectiveness and acceptability of the FDA-licensed proton pump inhibitors for erosive esophagitis: a PRISMA-compliant network meta-analysis. Medicine (Baltimore). 2017;96(39):e8120.
Ali, M., el Chaar M., Ghiassi S., Rogers A.M., American Society for Metabolic and Bariatric Surgery Clinical Issues Committee., American Society for Metabolic and Bariatric Surgery updated position statement on sleeve gastrectomy as a bariatric procedure. Surg Obes Relat Dis, 2017. 13(10): p. 1652–1657.
Quezada N, Hernández J, Pérez G, et al. Laparoscopic sleeve gastrectomy conversion to Roux-en-Y gastric bypass: experience in 50 patients after 1 to 3 years of follow-up. Surg Obes Relat Dis. 2016;12(8):1611–5.
Jones Jr KB. Roux-en-Y gastric bypass: an effective antireflux procedure in the less than morbidly obese. Obes Surg. 1998;8(1):35–8.
Smith SC, Edwards CB, Goodman GN. Symptomatic and clinical improvement in morbidly obese patients with gastroesophageal reflux disease following Roux-en-Y gastric bypass. Obes Surg. 1997;7(6):479–84.
Perry, Y., et al., Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. Jsls, 2004. 8(1): p. 19–23.
Namikawa T, Kitagawa H, Okabayashi T, et al. Roux-en-Y reconstruction is superior to billroth I reconstruction in reducing reflux esophagitis after distal gastrectomy: special relationship with the angle of his. World J Surg. 2010;34(5):1022–7.
Berger EH. The distribution of parietal cells in the stomach: a histotopographic study. Am J Anat. 1934;54(1):87–114.
Smith CD, Herkes SB, Behrns KE, et al. Gastric acid secretion and vitamin B12 absorption after vertical roux-en-Y gastric bypass for morbid obesity. Ann Surg. 1993;218(1):91–6.
Fein M et al. Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. J Gastrointest Surg. 1999;3(4):405–10.
van Herwaarden MA, Samsom M, Smout AJ. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology. 2000;119(6):1439–46.
Kahrilas PJ, Shi G, Manka M, et al. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gastroenterology. 2000;118(4):688–95.
Gulkarov I, Wetterau M, Ren CJ, et al. Hiatal hernia repair at the initial laparoscopic adjustable gastric band operation reduces the need for reoperation. Surg Endosc. 2008;22(4):1035–41.
Kahrilas PJ. The role of hiatus hernia in GERD. The Yale J Biol Med. 1999;72(2–3):101–11.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Barham K. Abu Dayyeh reports personal fees from USGI Medical, grants from Apollo Endosurgery, personal fees from Johnson and Johnson, personal fees from Olympus, grants and personal fees from Boston Scientific, during the conduct of the study. Other authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by institutional IRB.
Informed Consent
For this type of study, formal consent was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matar, R., Maselli, D., Vargas, E. et al. Esophagitis After Bariatric Surgery: Large Cross-sectional Assessment of an Endoscopic Database. OBES SURG 30, 161–168 (2020). https://doi.org/10.1007/s11695-019-04164-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04164-0