Abstract
Objective
Weight outcomes after bariatric surgery are due to an adequate adjustment of eating behavior to the new gastrointestinal conditions created by operation. The efficacy of dietary/behavior counseling for promoting weight loss and maintenance in a growing number of bariatric patients was investigated.
Material and Methods
One hundred seventy-six non-diabetic obese patients undergoing Roux-en-Y gastric bypass (RYGBP) and sleeve gastrectomy (SG) were investigated. The first group (CO, 88 subjects, 16 male) attended a standard surgical follow-up, while in the second (DIET, 88 subjects, 15 male) the surgeon was supported by a dietitian, and patients received behavioral-dietary sessions on individual request. Data prior to the operation and at 2 years were considered, the weight outcome being regarded as successful when postoperative body mass index (BMI) value was lower than 30 kg/m2.
Results
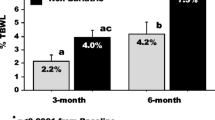
Weight results were better (p < 0.01) in the RYGBP than in the SG patients. In comparison to CO, in the DIET group a greater adherence to the bariatric program was observed (76% vs. 41%, < 0.01), while body weight data and prevalence of successful cases at 2 years (87 ± 23 vs. 83 ± 16 kg and 27% vs.33%, respectively) were similar.
Conclusions
After RYSG and SG, postoperative dietetic/behavioral sessions delivered on patient’s request does not influence weight results. The dietetic intervention promotes the adherence to bariatric program and prevents postoperative follow-up loss. In a dietitian/behavioral strategy after RYGBP and SG, a cognitive reinforcement of the compliance to bariatric program and a strengthening of the motivation to changes could promote better weight results.

Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Puzziferri N, Roshek 3rd TB, Mayo HG, et al. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014;312(9):934–42.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Cardoso L, Rodrigues D, Gomes L, et al. Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab. 2017;19(9):1223–32.
Sjöström L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65.
Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016;26(11):2590–601.
de Zwaan M, Hilbert A, Swan-Kremeier L, et al. Comprehensive interview assessment of eating behavior 18-35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6(1):79–85.
Sarwer DB, Dilks RJ, West-Smith L. Dietary intake and eating behavior after bariatric surgery: threats to weight loss maintenance and strategies for success. Surg Obes Relat Dis. 2011;7(5):644–51.
Pizato N, Botelho PB, Gonçalves VSS, Dutra ES, de Carvalho KMB. Effect of grazing behavior on weight regain post-bariatric surgery: a systematic review. Nutrients 2017;9(12).
Al-Najim W, Docherty NG, le Roux CW. Food intake and eating behavior after bariatric surgery. Physiol Rev. 2018;98(3):1113–41.
Sharples AJ, Mahawar K, Cheruvu CVN. Systematic review and retrospective validation of prediction models for weight loss after bariatric surgery. Surg Obes Relat Dis. 2017;13(11):1914–20.
Hindle A, de la Piedad GX, Brennan L. Early post-operative psychosocial and weight predictors of later outcome in bariatric surgery: a systematic literature review. Obes Rev. 2017;18(3):317–34.
Rudolph A, Hilbert A. Post-operative behavioural management in bariatric surgery: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2013;14(4):292–302.
Andromalos L, Crowley N, Brown J, et al. Nutrition care in bariatric surgery: an academy evidence analysis center systematic review. J Acad Nutr Diet. 2019;119(4):678–86.
Song Z, Reinhardt K, Buzdon M, et al. Association between support group attendance and weight loss after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2008;4(2):100–3.
Kaiser KA, Franks SF, Smith AB. Positive relationship between support group attendance and one-year postoperative weight loss in gastric banding patients. Surg Obes Relat Dis. 2011;7(1):89–93.
Nijamkin MP, Campa A, Sosa J, et al. Comprehensive nutrition and lifestyle education improves weight loss and physical activity in Hispanic Americans following gastric bypass surgery: a randomized controlled trial. J Acad Nutr Diet. 2012;112(3):382–90.
Hildebrandt SE. Effects of participation in bariatric support group after Roux-en-Y gastric bypass. Obes Surg. 1998;8(5):535–42.
Sarwer DB, Moore RH, Spitzer JC, et al. A pilot study investigating the efficacy of postoperative dietary counseling to improve outcomes after bariatric surgery. Surg Obes Relat Dis. 2012;8(5):561–8.
El Chaar M, McDeavitt K, Richardson S, et al. Does patient compliance with preoperative bariatric office visits affect postoperative excess weight loss? Surg Obes Relat Dis. 2011;7(6):743–8.
Galioto R, Gunstad J, Heinberg LJ, et al. Adherence and weight loss outcomes in bariatric surgery: does cognitive function play a role? Obes Surg. 2013;23(10):1703–10.
Kim HJ, Madan A, Fenton-Lee D. Does patient compliance with follow-up influence weight loss after gastric bypass surgery? A systematic review and meta-analysis. Obes Surg. 2014;24(4):647–51.
Lager CJ, Esfandiari NH, Subauste AR, et al. Roux-en-Y Gastric bypass vs. Sleeve gastrectomy: balancing the risks of surgery with the benefits of weight loss. Obes Surg. 2017;27(1):154–61.
Yang P, Chen B, Xiang S, Lin XF, Luo F, Li W. Long-term outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for morbid obesity: results from a meta-analysis of randomized controlled trials. Surg Obes Relat Dis 2019
le Roux CW, Welbourn R, Werling M, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246(5):780–5.
Malin SK, Kashyap SR. Differences in weight loss and gut hormones: Rouen-Y gastric bypass and sleeve gastrectomy surgery. Curr Obes Rep. 2015;4(2):279–86.
Benaiges D, Más-Lorenzo A, Goday A, et al. Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol. 2015;21(41):11804–14.
Conceição EM, Utzinger LM, Pisetsky EM. Eating disorders and problematic eating behaviours before and after bariatric surgery: characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev. 2015;23:417–25.
de Zwaan M, Hilbert A, Swan-Kremeier L, et al. Comprehensive interview assessment of eating behavior 18–35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6:79–85.
Burgmer R, Grigutsch K, Zipfel S, et al. The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg. 2005;15:684–91.
Poole NA, Al Atar A, Kuhanendran D, et al. Compliance with surgical after-care following bariatric surgery for morbid obesity: a retrospective study. Obes Surg. 2005;15(2):261–5.
te Riele WW, Boerma D, Wiezer MJ, et al. Long-term results of laparoscopic adjustable gastric banding in patients lost to follow-up. Br J Surg. 2010;97(10):1535–40.
Júnior WS, Do Amaral JL, Nonino-Borges CB. Factors related to weight loss up to 4 years after bariatric surgery. Obes Surg. 2011;21(11):1724–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gradaschi, R., Molinari, V., Sukkar, S.G. et al. Effects of the Postoepartive Dietetic/Behavioral Counseling on the Weight Loss After Bariatric Surgery. OBES SURG 30, 244–248 (2020). https://doi.org/10.1007/s11695-019-04146-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04146-2