Abstract
Introduction
Although bariatric surgery promotes dietary changes, many questions regarding their effect on weight loss remain unanswered.
Objective
The aim of this study was to evaluate changes in dietary intake and predictive factors of obesity remission in the first 12 months after RYGB.
Methods
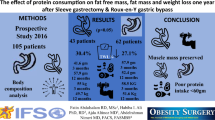
Fifty-one patients (mean 39.34 ± 9.38 years, 68.7% women) who underwent RYGB were included in this study. Dietary intake was evaluated through a 24-h dietary recall and subsequently classified by NOVA, macronutrients and calories. The predictive factors for obesity remission within 12 months after RYGB were evaluated by Cox regression.
Results
At baseline, 62.7% of the patients presented severe obesity; mean excess weight loss was greater than 80% after 1 year of surgery and about 70% of the patients were no longer diagnosed with obesity. An increase in percentage of calories from protein was observed at 3 and 12 months after surgery. The caloric contribution of ultra-processed foods was low at 3 months after surgery while that of unprocessed or minimally processed foods was high at 3 and 12 months after surgery. From the Cox regression analysis, preoperative BMI (HR, 0.78; 95% CI, 0.69–0.88) and age (HR, 0.94; 95% CI, 0.89–0.99) showed an inverse association with obesity remission. Also, Δ protein (at 3 months–baseline) showed a positive association with obesity remission (HR, 1.06; 95% CI, 1.01–1.12).
Conclusion
Lower preoperative BMI, lower age, and higher protein intake at 3 months after surgery may favor remission of obesity in up to 12 months compared with baseline.
Similar content being viewed by others
References
Laurenius A, Larsson I, Bueter M, et al. Changes in eating behaviour and meal pattern following Roux-en-Y gastric bypass. Int J Obes. 2012;36:348–55.
Golzarand M, Toolabi K, Djafarian K. Changes in body composition, dietary intake, and substrate oxidation in patients underwent laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy: a comparative prospective study. Obes Surg. 2018;29(2):406–13.
Gero D, Steinert RE, le Roux CW, et al. Do food preferences change after bariatric surgery? Curr Atheroscler Rep. 2017;19(9):31–8.
Pinto SL, Cristina D, Bressan J. Absolute and relative changes in ultra-processed food consumption and dietary antioxidants in severely obese adults 3 months after Roux-en-Y gastric bypass. Obes Surg. 2019;29(6):1810–5.
Ahmed K, Penney N. Taste changes after bariatric surgery : a systematic review. Obes Surg. 2018;28:3321–32.
Boerlage TCC, Van de Laar AWJM, Westerlaken S, et al. Gastrointestinal symptoms and food intolerance 2 years after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Br J Surg. 2017;104:393–400.
Mechanick JI, Kushner RF, Sugerman HJ, et al. Guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr Pract. 2008;14:1–83.
Louzada ML d C, Baraldi LG, Steele EM, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15.
Juul F, Martinez-Steele E, Parekh N, et al. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120:90–100.
Louzada ML d C, Martins APB, Canella DS, et al. Ultra-processed foods and the nutritional dietary profile in Brazil. Rev Saude Publica. 2015;49:1–11.
Lissner L, Lindroos AK, Sjöström L. Swedish obese subjects (SOS): an obesity intervention study with a nutritional perspective. Eur J Clin Nutr. 1998;52:316–22.
Miller GD, Norris A, Fernandez A. Changes in nutrients and food groups intake following laparoscopic Roux-en-Y gastric bypass (RYGB). Obes Surg. 2014;24:1926–32.
Subramaniam K, Low W, Lau P, et al. Eating behaviour predicts weight loss six months after bariatric surgery: a longitudinal study. Nutrients. 2018;10:1616.
Barufaldi LA, Abreu G de A, da VGV, et al. Programa para registro de recordatório alimentar de 24 horas: aplicação no Estudo de Riscos Cardiovasculares em Adolescentes. Rev Bras Epidemiol. 2016;19:464–8.
IBGE. Brazilian Institute of Geography and Statistics - Family Budget Research: 2008–2009.Analysis of personal food consumption in Brazil. Bibl of the Ministry Planning, Budget and Management 2011.
Monteiro CA, Cannon G, Moubarac JC, et al. The UN decade of nutrition, the NOVA food classification and the trouble with ultraprocessing. Public Health Nutr. 2018;21:5.
Monteiro CA, Moubarac JC, Cannon G, et al. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8.
Jellife D. Evoluación del estado nutricion dela comunidad. Ginebra, OMS. Série Monogr. 1968;53
World Health Organization. World Health Statistics 2010. World Health 2010; 177.
Poti JM, Braga B, Qin B. Ultra-processed food intake and obesity: what really matters for health-processing or nutrient content? Curr Obes Rep. 2017;6:420–31.
Buchwald H. Consensus Conference Statement Bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005;1:371–81.
Rodrigues GK, Resende CMM, Durso DF, et al. A single FTO gene variant rs9939609 is associated with body weight evolution in a multiethnic extremely obese population that underwent bariatric surgery. Nutrition. 2015;31:1344–50.
Ortega E, Morínigo R, Flores L, et al. Predictive factors of excess body weight loss 1 year after laparoscopic bariatric surgery. Surg Endosc. 2012;26:1744–50.
Kanerva N, Larsson I, Peltonen M, et al. Changes in total energy intake and macronutrient composition after bariatric surgery predict long-term weight outcome: findings from the Swedish Obese Subjects (SOS) study. Am J Clin Nutr. 2017;106:136–45.
Westerterp-Plantenga MS, Nieuwenhuizen A, Tomé D, et al. Dietary protein, weight loss, and weight maintenance. Annu Rev Nutr. 2009;29:21–41.
Veldhorst M, Smeets A, Soenen S, et al. Protein-induced satiety: effects and mechanisms of different proteins. Physiol Behav. 2008;94:300–7.
Laurenius A, Larsson I, Melanson KJ, et al. Decreased energy density and changes in food selection following Roux-en-Y gastric bypass. Eur J Clin Nutr. 2013;67:168–73.
Acknowledgments
We thank all the volunteers in the research.
Funding
This project is funded by the Coordination for the Improvement of Personnel (CAPES).
Author information
Authors and Affiliations
Contributions
SLP: Contributed in the design of the study, data collection, analysis and interpretation, manuscript writing, and final version approval.
LLJ and JB: Contributed in the design of the study, analysis and interpretation of the data, critical revision of the manuscript, and approval of the final version.
Corresponding author
Ethics declarations
All the patients signed an informed consent form (ICF) accepting to participate in the project. The study was approved by the Ethics and Research Committee (CEP) of the Federal University of Viçosa (no. 1.852.365).
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pinto, S.L., Juvanhol, L.L. & Bressan, J. Increase in Protein Intake After 3 Months of RYGB Is an Independent Predictor for the Remission of Obesity in the First Year of Surgery. OBES SURG 29, 3780–3785 (2019). https://doi.org/10.1007/s11695-019-04124-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-04124-8