Abstract
Background
Patients undergoing Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) have different healthcare needs after surgery. Our aim was to quantify non-routine healthcare utilization after RYGB vs. SG.
Methods
We compared non-routine (NR) visits made and associated services provided up to 2 years post-surgery for patients undergoing RYGB or SG at a Bariatric Surgery Comprehensive Center between March 2013 and April 2015.
Results
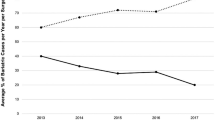
A total of 258 and 461 patients had primary RYGB and SG, respectively. Successful follow-up rates at one (76.2%) and 2 years post-surgery (52.6%) did not differ between groups. Rates for all NR visits, expressed as the number per 100 patients, were 68.6 in RYGB vs. 35.4 in SG patients (p < 0.0001). Emergency department visits with subsequent admission (EDA) or without subsequent admission (ED-only) and outpatient visits (OPV) were more frequent in RYGB vs. SG: EDA, 14.7 vs. 8.0 (p = 0.0076); ED-only, 17.8 vs. 7.6 (p = 0.0001); and OPV, 29.8 vs. 14.1 (p < 0.0001). RYGB required more services per 100 patients than SG, 120.9 vs. 75.3, respectively (p < 0.0001). Imaging was the resource most often used overall. Surgery type (RYGB) significantly predicted healthcare utilization even after controlling for gender, ethnicity, and other variables. Healthcare utilization peaked at 1 to 6 months post-surgery, driven by patients who underwent RYGB.
Conclusions
RYGB required twice as many non-routine follow-up visits and 1.6 times greater use of healthcare services relative to SG. Computer-assisted tomography imaging and endoscopies showed the greatest differences. Peak healthcare utilization for RYGB occurred between 1 and 6 months following surgery.

Similar content being viewed by others
References
Al-Khyatt W, Ryall R, Leeder P, et al. Predictors of inadequate weight loss after laparoscopic gastric bypass for morbid obesity. Obes Surg. 2016.
Lee JH, Nguyen QN, Le QA. Comparative effectiveness of 3 bariatric surgery procedures: Roux-en-Y gastric bypass, laparoscopic adjustable gastric band, and sleeve gastrectomy. Surg Obes Relat Dis. 2016;12:997–1002.
Zhang C, Yuan Y, Qiu C, et al. A meta-analysis of 2-year effect after surgery: laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for morbid obesity and diabetes mellitus. Obes Surg. 2014;24:1528–35.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2016;26:429–42.
Bohdjalian A, Langer FB, Shakeri-Leidenmuhler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–40.
Langer FB, Bohdjalian A, Shakeri-Leidenmuhler S, et al. Conversion from sleeve gastrectomy to Roux-en-Y gastric bypass--indications and outcome. Obes Surg. 2010;20:835–40.
Toussi R, Fujioka K, Coleman KJ. Pre- and postsurgery behavioral compliance, patient health, and postbariatric surgical weight loss. Obesity (Silver Spring). 2009;17:996–1002.
Elms L, Moon RC, Varnadore S, et al. Causes of small bowel obstruction after Roux-en-Y gastric bypass: a review of 2,395 cases at a single institution. Surg Endosc. 2014;28:1624–8.
Lee WJ, Pok EH, Almulaifi A, et al. Medium-term results of laparoscopic sleeve gastrectomy: a matched comparison with gastric bypass. Obes Surg. 2015;25:1431–8.
Zaveri H, Dallal RM, Cottam D, et al. Indications and operative outcomes of gastric bypass reversal. Obes Surg. 2016;26:2285–90.
Li JF, Lai DD, Lin ZH, et al. Comparison of the long-term results of Roux-en-Y gastric bypass and sleeve gastrectomy for morbid obesity: a systematic review and meta-analysis of randomized and nonrandomized trials. Surg Laparosc Endosc Percutan Tech. 2014;24:1–11.
Carlin AM, Zeni TM, English WJ, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013;257:791–7.
Hutter JCMM. The MBSAQIP (Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program) Comprehensive Bariatric Program (MBSAQIP-ASMBS/ACS). The SAGES Manual of Bariatric Surgery; 2017. p. 185–90.
Garg T, Rosas U, Rogan D, et al. Characterizing readmissions after bariatric surgery. J Gastrointest Surg. 2016;20:1797–801.
Hutter MM, Schirmer BD, Jones DB, et al. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg. 2011;254:410–20. discussion 20-2
Mora-Pinzon MC, Henkel D, Miller RE, et al. Emergency department visits and readmissions within 1 year of bariatric surgery: a statewide analysis using hospital discharge records. Surgery. 2017;162:1155–62.
Sahai H, Kuhurshid A. Statistics in epidemiology: methods, techniques, and applications. Boca Raton: CRC Press, Inc.; 1996.
Haddad D, David A, Abdel-Dayem H, et al. Abdominal imaging post bariatric surgery: predictors, usage and utility. Surg Obes Relat Dis. 2017;13:1327–36.
Li K, Gao F, Xue H, et al. Comparative study on laparoscopic sleeve gastrectomy and laparoscopic gastric bypass for treatment of morbid obesity patients. Hepatogastroenterology. 2014;61:319–22.
American College of Emergency Physicians. Bariatric examination, assessment and management. Avaliable at https://www.acep.org/patient-care/beam/#sm.00ik7too14bwfhg10x718i2hytwr1. Accessed 15 Oct 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study site is accredited by the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). The study was approved by the local Institutional Review Board.
Conflict of Interest
DT served as a consultant for Olympus and Medtronic. PP served as a consultant for Olympus.
Statement of Informed Consent
This study was approved by the Hartford Hospital Institutional Review Board (HHC-2017-0077) with a waiver of informed consent.
Ethical Approval
This study was approved by the Hartford Hospital Institutional Review Board (HHC-2017-0077). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seip, R.L., Robey, K., Stone, A. et al. Comparison of Non-routine Healthcare Utilization in the 2 years Following Roux-En-Y Gastric Bypass and Sleeve Gastrectomy: A Cohort Study. OBES SURG 29, 1922–1931 (2019). https://doi.org/10.1007/s11695-019-03793-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03793-9