Abstract
Introduction
Obesity is one of the greatest health problems. Bariatric surgery is more effective than non-surgical options; however, postoperative pain is bound to a greater morbidity. Control of postoperative pain is important in facilitating patient convalescence. In this study, we assessed the efficacy of intraperitoneal instillation of bupivacaine after bariatric surgery.
Methods
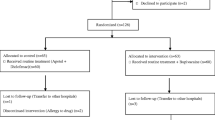
A hundred patients who underwent bariatric procedures including sleeve gastrectomy, sleeve gastrectomy with cardioplasty, gastric bypass, and gastric mini bypass (one anastomosis gastric bypass) were included in the study. Patients were divided into two groups randomly, 50 patients for each; group I had intraperitoneal instillation of 40 ml bupivacaine 0.25% at the end of the procedure, while group II had normal saline instillation. Monitoring of pain control in the first 24 h after surgery was done using the visual analogue scale (VAS) to assess the efficacy of intraperitoneal bupivacaine instillation and its effect on the overall opioid usage, postoperative nausea and vomiting (PONV), and shoulder tip pain.
Results
Pain scores were significantly lower in group I compared to group II at recovery, 2, 4 and 6 h after surgery, P = 0.004, 0.001, < 0.001, and 0.001 respectively. However, there were no significant differences between 12 and 24 h postoperatively. Additionally, there was a significant difference regarding the need for rescue analgesia at recovery P = < 0.001*. Further analysis revealed lower morphine consumption via PCA in group I compared to group II P = 0.013*. There were no significant differences with the use of intraperitoneal bupivacaine as regards nausea, vomiting, or shoulder tip pain, P = 0.688, 0.249, and 0.487, respectively.
Conclusions
Intraperitoneal instillation of bupivacaine provides a good analgesia in the early postoperative period, reduces the overall consumption of opioid, and decreases the rescue analgesia requirement in the first 24 h after surgery.


Similar content being viewed by others
References
Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9:13–27.
Yan LL, Daviglus ML, Liu K, et al. Midlife body mass index and hospitalization and mortality in older age. JAMA. 2006;295:190–8.
Vlad I. Obesity costs UK economy 2bn pounds sterling a year. BMJ. 2003;327:1308.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Zhou X, Yu J, Li L, et al. Effects of bariatric surgery on mortality, cardiovascular events, and cancer outcomes in obese patients: systematic review and meta-analysis. Obes Surg. 2016 Nov;26(11):2590–601. https://doi.org/10.1007/s11695-016-2144-x.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61.
Babu R, Jain P, Sherif L. Intraperitoneal instillation: ropivacaine vs bupivacaine for post operative pain relief in laparoscopic cholecystectomy. Int J Health Sci Res. 2013;3(12):42–7.
Rawal N, Allvin R, Amilon A. Postoperative analgesia at home after ambulatory hand surgery: a controlled comparison of tramadol, metamizole and paracetamol. Anesth Analg. 2001;92:347–51.
Egan TD. Miller’s anesthesia. 6th ed. Anesthesiology 2005;103(3):673.
Bisgaard T, Klarskov B, Rosenberg J, et al. Characteristics and prediction of early pain after laparoscopic cholecystectomy. Pain. 2001;90(3):261–9.
Kandil TS, El Hefnawy E. Shoulder pain following laparoscopic cholecystectomy: factors affecting the incidence and severity. J Laparoendosc Adv Surg Tech A. 2010;20(8):677–82.
Tolver MA, Strandfelt P, Rosenberg J, et al. Pain characteristics after laparoscopic inguinal hernia repair. Surg Endosc. 2011;25(12):3859–64.
Bisgaard T, Stockel M, Klarskov B, et al. Prospective analysis of convalescence and early pain after uncomplicated laparoscopic fundoplication. Br J Surg. 2004;91(11):1473–8.
American Society of Hospital Pharmacists, Committee on Pharmacy and Pharmaceuticals. American hospital formulary service; a collection of drug monographs and other information. Hamilton: Hamilton Press; 1996.
Fernandez AZ, Demaria EJ, Tichansky DS, et al. Multivariate analysis of risk factors for death following gastric bypass for treatment of morbid obesity. Ann Surg. 2004;239:698–703.
Huang S, Mi S, He Y, et al. Analgesic efficacy of trocar sites local anaesthetic infiltration with and without transversus abdominis plane block after laparoscopic hysterectomy: a randomized trial. Int J Clin Exp Med. 2016;9(3):6518–24.
Yadava A, Rajput SK, Katiyar S, et al. A comparison of intraperitoneal bupivacaine – tramadol with bupivacaine – magnesium sulphate for pain relief after laparoscopic cholecystectomy: prospective, randomised study. Indian J Anaesth. 2016;60(10):757–62.
Badawy AM. Intraperitoneal analgesia to reduce pain after laparoscopic hysterectomy. Int J Reprod Contracept Obstet Gynecol. 2017;6:3235–40.
Kim AJ, Yong RJ, Urman RD. The role of transversus abdominis plane blocks in ERAS pathways for open and laparoscopic colorectal surgery. J Laparoendosc Adv Surg Tech A. 2017 Published online 2017 Jul 25;27:909–14. https://doi.org/10.1089/lap.2017.0337.
Oh TK, Lee SJ, Do SH, et al. Transversus abdominis plane block using a short-acting local anaesthetic for postoperative pain after laparoscopic colorectal surgery: a systematic review and meta-analysis. Surg Endosc. 2018;32(2):545–52.
Hamill JK, Rahiri JL, Hill AG. Analgesic effect of intraperitoneal local anaesthetic in surgery: an overview of systematic reviews. J Surg Res. 2017;212:167–77. https://doi.org/10.1016/j.jss.2017.01.022.
Scarth E, Smith S. Drugs in anaesthesia and intensive care. 5th ed. Oxford University Press; 2016. https://doi.org/10.1093/med/9780198768814.001.0001.
Malhotra N, Chanana C, Roy KK, et al. To compare the efficacy of two doses of intraperitoneal bupivacaine for pain relief after operative laparoscopy in gynaecology. Arch Gynecol Obstet. 2007;276(4):323–6.
Mitra S, Khandelwal P, Roberts K, et al. Pain relief in laparoscopic cholecystectomy--a review of the current options. Pain Pract. 2012;12(6):485–96.
Kahokehr A, Sammour T, Srinivasa S, et al. Systematic review and meta-analysis of intraperitoneal local anaesthetic for pain reduction after laparoscopic gastric procedures. Br J Surg. 2011;98(1):29–36.
Marks JL, Ata B, Tulandi T. Systematic review and meta-analysis of intraperitoneal instillation of local anaesthetics for reduction of pain after gynecologic laparoscopy. J Minim Invasive Gynecol. 2012;19(5):545–53.
Ruiz-Tovar J, Gonzalez J, Garcia A, et al. Intraperitoneal Ropivacaine irrigation in patients undergoing bariatric surgery: a prospective randomized clinical trial. Obes Surg. 2016 Nov;26(11):2616–21.
Cohen AR, Smith AN, Henriksen BS. Postoperative opioid requirements following Roux-en-Y gastric bypass in patients receiving continuous bupivacaine through a pump system: a retrospective review. Hosp Pharm. 2013;48(6):479–83.
Bindra TK, Chawla D, Kumar P, et al. Comparison of intraperitoneal instillation of ropivacaine with normal saline in laparoscopic cholecystectomy. Int J Res Med Sci. 2017;5:4924–8.
Choi GJ, Kang H, Baek CW, et al. Effect of intraperitoneal local anaesthetic on pain characteristics after laparoscopic cholecystectomy. World J Gastroenterol. 2015;21(47):13386–95.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Approved by the ethical committee.
Consent
Written informed consent was obtained from the patient for participation in the study before allocation to either arms of the study, in addition to publishing the results.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Omar, I., Abualsel, A. Efficacy of Intraperitoneal Instillation of Bupivacaine after Bariatric Surgery: Randomized Controlled Trial. OBES SURG 29, 1735–1741 (2019). https://doi.org/10.1007/s11695-019-03775-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03775-x