Abstract
Introduction
Patients that undergo Roux-en-Y gastric bypass (RYGB) experience a dramatic change in food consumption; however, it is unknown whether food consumption changes in relation to the level of food processing.
Objective
The aim of this work was to evaluate the relationship between ultra-processed food intake, dietary antioxidant capacity, and cardiometabolic risk factors in patients who underwent RYGB.
Methods
This study included 58 obese patients who underwent RYGB bariatric surgery. Data collection was done pre-operatively and at 3 months post-surgery. The foods consumed were documented using a 3-day 24-h dietary recall, and food intake was classified based on NOVA and dietary total antioxidant capacity (TAC). Anthropometric and biochemical data as well as information on body composition were also collected. Metabolic syndrome (MS) was classified in accordance with the International Diabetes Federation.
Results
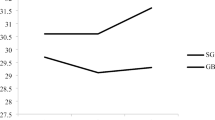
Ultra-processed foods amounted to 27.2% and 19.7% of the total calories consumed during pre- and post-surgery periods, respectively. Regarding post-surgery, the caloric contribution of unprocessed or minimally processed foods increased, from 55.7 to 70.2% (p = 0.000). The TAC of foods consumed is inversely proportional to that of ultra-processed foods. Obvious changes were observed in all the anthropometric variables, lipid profile, glycemia, insulin resistance, and MS.
Conclusion
Our results indicate that bariatric surgery is able to promote improvement in the diet quality of patients, reducing the consumption of ultra-processed foods and increasing the intake of unprocessed foods. The TAC of foods consumed is inversely proportional to that of ultra-processed ones.
Similar content being viewed by others
References
Bhurosy T, Kaschalk E, Smiley A, et al. Comment on “ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-up (SUN) cohort study”. Am J Clin Nutr. 2017;105:1012.1–012.
Canella DS, Levy RB, Paula A, et al. Ultra-processed food products and obesity in Brazilian households (2008–2009). PLoS One. 2014;9:1–6.
Marrón-Ponce JA, Sánchez-Pimienta TG, Da Costa Louzada ML, et al. Energy contribution of NOVA food groups and sociodemographic determinants of ultra-processed food consumption in the Mexican population. Public Health Nutr. 2018;21:87–93.
Monteiro CA, Cannon G, Moubarac JC, et al. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21:5–17.
Mozaffarian D, Hao T, Rimm EB, et al. Changes in diet and lifestyle and long-term weight gain in women and men. NIH Public Access. 2011;364:2392–404.
Monteiro CA, Moubarac JC, Cannon G, et al. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8.
O’Halloran SA, Lacy KE, Grimes CA, et al. A novel processed food classification system applied to Australian food composition databases. J Hum Nutr Diet. 2017;30:534–41.
Moubarac J, Batal M, Louzada ML, et al. Consumption of ultra-processed foods predicts diet quality in Canada. Appetite. 2016;108:512–20.
Nasreddine L, Tamim H, Itani L, et al. A minimally processed dietary pattern is associated with lower odds of metabolic syndrome among Lebanese adults. Public Health Nutr. 2018;21:160–71.
Fiolet T, Srour B, Sellem L, et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322.
Ahmed K, Penney N. Taste changes after bariatric surgery: a systematic review. Obes Surg. 2018;28(10):3321–32.
Lopez RPS & Botelho RBA. Photo album of food portions. Metha, Editor. 2008.
Barufaldi LA, de Abreu G, A, de Veiga GV, et al. Software to record 24-hour food recall: application in the study of cardiovascular risks in adolescents. Rev Bras Epidemiol. 2016;19:464–8.
IBGE. Brazilian Institute of Geography and Statistics - Family Budget Research: 2008–2009. Analysis of personal food consumption in Brazil. Bibl. of the Ministry. Planning, Budget and Management. 2011.
Jellife DB. The assessment of the nutritional status of the community. Geneva: WHO; 1966.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consulation. Geneva: WHO; 1998. Technical Report Series, 894.
Callaway CW. et al. Circumferences. Apud Lohman, TG; Roche, AF; Martorell, R. Anthropometric standarization reference manual. Champaign (IL): Human Kinetics.1988; 39–54.
Ben-Noun L, Laor A. Relationship of neck circumference to cardiovascular risk factors. Obes Res. 2003;11:226–31.
Matthews DR, Hosker JP, Rudenski a S, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Alberti KGMM, Zimmet PSJ. Metabolic syndrome-a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med. 2006;23:469–80.
Carlsen MH, Halvorsen BL, Holte K, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr J. 2010;9:1–11.
Zerrweck C, Zurita L, Álvarez G, et al. Taste and olfactory changes following laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg. 2016;26:1296–302.
Louzada ML d C, Baraldi LG, Steele EM, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med (Baltim) Elsevier Inc. 2015;81:9–15.
Juul F, Martinez-Steele E, Parekh N, et al. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120:90–100.
Graham L, Murty G, Bowrey DJ. Taste, smell and appetite change after Roux-en-Y gastric bypass surgery. Obes Surg. 2014;24:1463–8.
Olbers T, Björkman S, Lindroos A, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244:715–22.
Ernst B, Thurnheer M, Wilms B. Differential changes in dietary habits after gastric bypass versus gastric banding operations. Obes Surg. 2009;19:274–80.
Laurenius A, Larsson I, Bueter M, et al. Changes in eating behaviour and meal pattern following Roux-en-Y gastric bypass. Int J Obes. 2012;36:348–55.
Laurenius A, Larsson I, Melanson KJ, et al. Decreased energy density and changes in food selection following Roux-en-Y gastric bypass. Eur J Clin Nutr. 2013;67:168–73.
Batterham RL, Cummings DE. Mechanisms of diabetes improvement following bariatric/metabolic surgery. Diabetes Care. 2016;39:893–901.
Del Rio D, Agnoli C, Pellegrini N, et al. Total antioxidant capacity of the diet is associated with lower risk of ischemic stroke in a large Italian cohort. J Nutr. 2011;141:118–23.
Hollman PCH, Cassidy A, Comte B, et al. The biological relevance of direct antioxidant effects of polyphenols for cardiovascular health in humans is not established. J Nutr. 2011;141:989S–1009S.
Funding
This study was funded by the Coordination for the Improvement of Personnel at the CAPES.
Author information
Authors and Affiliations
Contributions
Sônia Lopes Pinto: contributed in the design of the study, data collection, analysis and interpretation, manuscript writing, and final version approval
Danielle Cristina Guimarães da Silva: contributed in the analysis and interpretation of the data, critical revision of the manuscript, and approval of the final version
Josefina Bressan: contributed in the design of the study, analysis and interpretation of the data, critical revision of the manuscript, and approval of the final version
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lopes Pinto, S., da Silva, D.C.G. & Bressan, J. Absolute and Relative Changes in Ultra-processed Food Consumption and Dietary Antioxidants in Severely Obese Adults 3 Months After Roux-en-Y Gastric Bypass. OBES SURG 29, 1810–1815 (2019). https://doi.org/10.1007/s11695-019-03749-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03749-z