Abstract
Background
Factors contributing to adolescents’ non-completion of bariatric surgery, defined as self-withdrawal during the preoperative phase of care, independent of program or insurance denial, are largely unknown. Recent adolescent and adult bariatric surgery literature indicate that psychological factors and treatment withdrawal play a role; however, for adolescents, additional age-salient (family/caregiver) variables might also influence progression to surgery.
Objectives
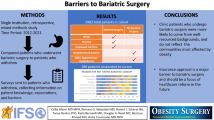
The present study examined demographic, psychological, and family/caregiver variables as predictors of whether adolescents completed surgery (“completers”) or withdrew from treatment (“non-completers”).
Setting
Adolescents were from a bariatric surgery program within a pediatric tertiary care hospital.
Methods
A retrospective chart review was conducted of consecutive patients who completed bariatric surgery psychological intake evaluations from September 2009 to April 2013. Data involving completer (n = 61) versus non-completer (n = 65) status were analyzed using two-tailed independent t tests, Chi-squared tests, and logistic regressions.
Results
Forty-three percent of adolescents completed surgery, similar to adult bariatric samples. Significantly more males were non-completers (p < .05), and there was a trend towards non-completion for older adolescents (p = 0.06). No other demographic, psychological, or caregiver/family variables were significant predictors of non-completion.
Conclusions
These findings indicate that demographic variables, rather than psychological or family factors, were associated with the progression to or withdrawal from surgery. Further assessment is needed to determine specific reasons for completing or withdrawing from treatment, particularly for males and older adolescents, to improve clinical care and reduce attrition.
Similar content being viewed by others
References
Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches. A scientific statement from the American Heart Association. Circulation. 2013;128:1689–712. https://doi.org/10.1161/CIR.0b013e3182a5cfb3.
Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999-2014. Obesity. 2016;24(5):1116–23. https://doi.org/10.1002/oby.21497.
Inge TH, Boyce TW, Lee M, et al. Access to care for adolescents seeking weight loss surgery. Obesity. 2014;22:2593–7. https://doi.org/10.1002/oby.20898.
Woolford SJ, Clark SJ, Sallinen BJ, et al. Bariatric surgery decision making challenges: the stability of teens’ decisions and the treatment failure paradox. PediatrSurgInt. 2012;28:455–60. https://doi.org/10.1007/s00383-012-3069-7.
Martin M, Beekley A, Kjorstad R, et al. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. SurgObesRelat Dis. 2010;6:8–15. https://doi.org/10.1016/j.soard.2009.07.003.
Sockalingam S, Cassin S, Crawford SA, et al. Psychiatric predictors of surgery non-completion following suitability assessment for bariatric surgery. ObesSurg. 2013;23:205–11. https://doi.org/10.1007/s11695-012-0762-5.
Merrell J, Ashton K, Windover A, et al. Psychological risk may influence drop-out prior to bariatric surgery. SurgObesRelat Dis. 2012;8:463–9. https://doi.org/10.1016/j.soard.2012.01.018.
Grave R, Calugi S, Molinari E, et al. Weight loss expectations in obese patients and treatment attrition: an observational multicenter study. Obes Res. 2005;13:1961–9. https://doi.org/10.1038/oby.2005.241.
Grossi E, Dalle Grave R, Mannucci, et al. Complexity of attrition in the treatment of obesity: clues from a structured telephone interview. Int J Obesity. 2006;30:1132–7. https://doi.org/10.1038/sj.ijo.0803244.
Moroshko I, Brennan L, O'Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12:912–34. https://doi.org/10.1111/j.1467-789x.2011.00915.x.
Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–70. https://doi.org/10.1016/j.jpeds.2003.12.031.
Cohen MJ, Curran JL, Phan TT, et al. Psychological contributors to noncompletion of an adolescent preoperative bariatric surgery program. SurgObesRelat Dis. 2017;13(1):58–64. https://doi.org/10.1016/j.soard.2016.08.020.
Zeller MH, Reiter-Purtill J. Psychosocial issues in adolescent bariatric surgery. In: The ASMBS Textbook of Bariatric Surgery. New York: Springer; 2014. p. 65–73. https://doi.org/10.1007/978-1-4939-1197-4_8.
Skelton JA, Goff DC, IP E, et al. Attrition in a multidisciplinary pediatric weight management clinic. Childhood Obesity. 2011;7(3):185–93. https://doi.org/10.1089/chi.2011.0010.
Schor EL. Family pediatrics: report of the task force on the family. Pediatrics. 2003;111:1541–71.
Skelton JA, Buehler C, Irby MB, et al. Where are family theories in family-based obesity treatment?: conceptualizing the study of families in pediatric weight management. Int J Obes. 2012;36(7):891–900. https://doi.org/10.1038/ijo.2012.56.
Zeller MH, Hunsaker S, Mikhail C, et al. Family factors that characterize adolescents with severe obesity and their role in weight loss surgery outcomes. Obesity. 2016;24:2562–9. https://doi.org/10.1002/oby.21676.
Skelton J, Beech B. Attrition in pediatric weight management: a review of the literature and new directions. Obes Rev. 2011;12:e273–81. https://doi.org/10.1111/j.1467-789x.2010.00803.x.
Gundersen, C, Mahatmya D, Garasky S, Lohman, B. Linking psychosocial stressors and childhood obesity. Obes Rev 2010; 12: e54-e63. https://doi.org/10.1111/j.1467-789x.2010.00813.x.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, revised. 4th ed.Washington DC: American Psychiatric Association; 2000. https://doi.org/10.1007/springerreference_179660.
Statistics IS SPSS version 21.0 for Microsoft windows platform. SPSS Inc.: Chicago, IL, USA, 2012.
Muthén LK, Muthén BO. Mplus version 7: Los Angeles, Muthén & Muthén; 1998-2014.
Santry HP, Gillen DL, Lauderdale DS. Trends in bariatric surgical procedures. JAMA. 2005;294:1909–17. https://doi.org/10.1001/jama.294.15.1909
Wee CC, Hamel MB, Apovian CM, et al. Expectations for weight loss and willingness to accept risk among patients seeking weight loss surgery. JAMA Surg. 2013;148(3):264–71. https://doi.org/10.1001/jamasurg.2013.1048
VerbruggeLM SRP. Physician treatment of men and women patients: sex bias or appropriate care? Med Care. 1981;19:609–32. https://doi.org/10.1097/00005650-198106000-00005
Tudiver F, Talbot Y. Why don’t men seek help? Family physicians’ perspective on help-seeking behavior in men. J Family Pract. 1999;48:47–52.
McQuaid EL, Kopel SJ, Klein RB, et al. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28:323–33. https://doi.org/10.1093/jpepsy/jsg022
Slotman GJ. Gastric bypass: a family affair—41 families in which multiple members underwent bariatric surgery. SurgObesRelat Dis. 2011;7:592–8. https://doi.org/10.1016/j.soard.2011.04.230
Zeller MH, Guilfoyle SM, Reiter-Purtil J, et al. Adolescent bariatric surgery: caregiver and family functioning across the first postoperative year. SurgObesRelat Dis. 2011;7:145–50. https://doi.org/10.1016/j.soard.2010.07.004
Inge TH, Zeller MH, Harmon CM, et al. Teen-longitudinal assessment of bariatric surgery: methodological features of the first prospective multicenter study of adolescent bariatric surgery. J PediatrSurg. 2007;42:1969–71. https://doi.org/10.1016/j.jpedsurg.2007.08.010
Sawhney P, Modi AC, Jenkins TM, et al. Predictors and outcomes of adolescent bariatric support group attendance. SurgObesRelat Dis. 2013;9:773–9. https://doi.org/10.1016/j.soard.2013.03.016
Cote MP, Byczkowski T, Kotagal U, et al. Service quality and attrition: an examination of a pediatric obesity program. Int J Qual Health Care. 2004;16(2):165–73. https://doi.org/10.1093/intqhc/mzh015
Kitscha CE, Brunet K, Farmer A, et al. Reasons for non-return to a pediatric weight management program. Can J Diet Prac Res. 2009;70(2):89–94. https://doi.org/10.3148/70.2.2009.89.
Sogg S, Lauretti J, West-Smith L. Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. SurgObesRelat Dis. 2016;12(4):731–49. https://doi.org/10.1016/j.soard.2016.02.008
Kizy S et al. National trends in bariatric surgery 2012–2015: demographics, procedure selection, readmissions, and cost. Obes Surg. 2017;27(11):2933–9. https://doi.org/10.1007/s11695-017-2719-1.
Acknowledgments
We acknowledge Linda Kollar, RN, MSN, CBN, Cassandra McDaniel, BA, Kathy Hrovat, MS, RD, LD, and Taylor Howarth, BA, for their contributions to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The current study received Institutional Review Board approval.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Formal consent is not required for data collection as part of routine clinical practice.
Statement of Human and Animal Rights
This study received institutional review board approval. All procedures performed were in accordance with institutional and national ethical standards of studies involving human participants.
Funding Agency
The first author was supported by a training grant from the National Institutes of Health (T32DK063929).
Rights and permissions
About this article
Cite this article
Brode, C., Ratcliff, M., Reiter-Purtill, J. et al. Predictors of Preoperative Program Non-Completion in Adolescents Referred for Bariatric Surgery. OBES SURG 28, 2853–2859 (2018). https://doi.org/10.1007/s11695-018-3261-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3261-5