Abstract
Introduction
Chronic liver disease is prevalent in obese patients presenting for bariatric surgery and is associated with increased postoperative morbidity and mortality (M&M). There are no comparative studies on the safety of different types of bariatric operations in this subset of patients.
Objective
The aim of this study is to compare the 30-day postoperative M&M between laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-Y-gastric bypass (LRYGB) in the subset of patients with a model of end-stage liver disease (MELD) score ≥ 8.
Methods
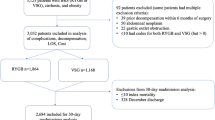
Data for LSG and LRYGB were extracted from the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database from years 2012 and 2013. MELD score was calculated using serum creatinine, bilirubin, INR, and sodium. Postoperative M&M were assessed in patients with a score ≥ 8 and compared for the type of operation. This was followed by analysis for MELD subcategories. Multiple logistic regression was performed to adjust for confounders.
Results
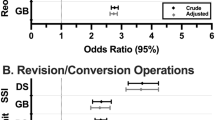
Out of 34,169, 9.8% of cases had MELD ≥ 8 and were included. Primary endpoint, 30-day M&M, was significantly lower post-LSG (9.5%) compared to LRYGB (14.7%); [AOR = 0.66(0.53, 0.83)]. Superficial wound infection, prolonged hospital stay, and unplanned readmission were more common in LRYGB. M&M post-LRYGB (30.6%) was significantly higher than LSG (15.7%) among MELD15-19 subgroup analysis.
Conclusion
LRYGB is associated with a higher postoperative risk than LSG in patients with MELD ≥ 8. The difference in postoperative complications between procedures was magnified with higher MELD. This suggests that LSG might be a safer option in morbidly obese patients with higher MELD scores, especially above 15.
Similar content being viewed by others
References
World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: WHO; 2014.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–14.
Clark JM. The epidemiology of nonalcoholic fatty liver disease in adults. Journal of clinical gastroenterology. 2006;40:S5–S10.
Angulo P. Nonalcoholic fatty liver disease. New England Journal of Medicine. 2002;346(16):1221–31.
Sasaki A, Nitta H, Otsuka K, et al. Bariatric surgery and non-alcoholic Fatty liver disease: current and potential future treatments. Frontiers in endocrinology. 2014;5:164.
Hannah Jr WN, Harrison SA. Effect of Weight Loss, Diet, Exercise, and Bariatric Surgery on Nonalcoholic Fatty Liver Disease. Clin Liver Dis. 2016;20(2):339–50.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient--2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis. 2013;9(2):159–91.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
Mathurin P, Hollebecque A, Arnalsteen L, et al. Prospective study of the long-term effects of bariatric surgery on liver injury in patients without advanced disease. Gastroenterology. 2009;137(2):532–40.
Mattar SG, Velcu LM, Rabinovitz M, et al. Surgically-induced weight loss significantly improves nonalcoholic fatty liver disease and the metabolic syndrome. Ann Surg. 2005;242(4):610.
Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003 Jan;124(1):91–6.
Goldberg DA, Gilroy R, Charlton M. New organ allocation policy in liver transplantation in the United States. Clin Liver Dis. 2016;8(4):108–12.
Ruf AE, Kremers WK, Chavez LL, et al. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transpl. 2005;11(3):336–43.
Suman A, Barnes DS, Zein NN, et al. Predicting outcome after cardiac surgery in patients with cirrhosis: a comparison of Child-Pugh and MELD scores. Clin Gastroenterol Hepatol. 2004;2(8):719–23.
Befeler AS, Palmer DE, Hoffman M, et al. The safety of intra-abdominal surgery in patients with cirrhosis: model for end-stage liver disease score is superior to Child-Turcotte-Pugh classification in predicting outcome. Arch Surg. 2005;140(7):650–4.
Farnsworth N, Fagan SP, Berger DH, et al. Child-Turcotte-Pugh versus MELD score as a predictor of outcome after elective and emergent surgery in cirrhotic patients. Am J Surg. 2004;188(5):580–3.
Krafcik BM, Farber A, Eslami MH, et al. The role of Model for End-Stage Liver Disease (MELD) score in predicting outcomes for lower extremity bypass. J Vasc Surg. 2016;64(1):124–30.
Zielsdorf SMMD, Kubasiak JCMD, Janssen IP, et al. A NSQIP Analysis of MELD and Perioperative Outcomes in General Surgery. Am Surg. 2015;81(8):755–9.
Elnahas A, Nguyen GC, Okrainec A, et al. The effect of underlying liver disease on short-term outcomes following bariatric surgery. Surg Endosc. 2014;28(9):2708–12.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. e5.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg. 2004;240(3):416.
Adams TD, Davidson LE, Litwin SE, et al. Health benefits of gastric bypass surgery after 6 years. Jama. 2012;308(11):1122–31.
Shiloach M, Frencher Jr SK, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6–16.
Clerical Changes for Implementation of Adding Serum Sodium to the MELD Score, Policy 9.1.D, (2016).
Dakour Aridi H, Alami R, Tamim H, et al. Long-term outcomes of laparoscopic sleeve gastrectomy: a Lebanese center experience. Surg Obes Relat Dis. 2016;12(9):1689–96.
Kehagias I, Karamanakos SN, Argentou M, et al. Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI< 50 kg/m2. Obes Surg. 2011;21(11):1650–6.
Rondelli F, Bugiantella W, Vedovati MC, et al. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy: a retrospective multicenter comparison between early and long-term post-operative outcomes. Int J Surg. 2017 Jan;37:36–41.
Mummadi RR, Kasturi KS, Chennareddygari S, et al. Effect of bariatric surgery on nonalcoholic fatty liver disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2008;6(12):1396–402.
Mosko JD, Nguyen GC. Increased perioperative mortality following bariatric surgery among patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9(10):897–901.
Dallal RM, Mattar SG, Lord JL, et al. Results of Laparoscopic Gastric Bypass in Patients with Cirrhosis. Obes Surg. 2004;14(1):47–53.
Shimizu H, Phuong V, Maia M, et al. Bariatric surgery in patients with liver cirrhosis. Surg Obes Relat Dis. 2013;9(1):1–6.
Pestana L, Swain J, Dierkhising R, et al. Bariatric surgery in patients with cirrhosis with and without portal hypertension: a single-center experience. Mayo Clin Proc. 2015;90(2):209–15.
Weingarten TN, Swain JM, Kendrick ML, et al. Nonalcoholic Steatohepatitis (NASH) does not increase complications after laparoscopic bariatric surgery. Obes Surg. 2011;21(11):1714–20.
Singh T, Kochhar GS, Goh GB, et al. Safety and efficacy of bariatric surgery in patients with advanced fibrosis. Int J Obes (Lond). 2017;41(3):443–9.
Sanni A, Perez S, Medbery R, et al. Postoperative complications in bariatric surgery using age and BMI stratification: a study using ACS-NSQIP data. Surg Endosc. 2014;28(12):3302–9.
Young MT, Gebhart A, Phelan MJ, et al. Use and outcomes of laparoscopic sleeve gastrectomy vs laparoscopic gastric bypass: analysis of the American College of Surgeons NSQIP. J Am Coll Surg. 2015;220(5):880–5.
Vidal P, Ramón JM, Goday A, et al. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy as a definitive surgical procedure for morbid obesity. Mid-term results. Obes Surg. 2013;23(3):292–9.
Carlin AM, Zeni TM, English WJ, et al. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann Surg. 2013;257(5):791–7.
Peterli R, Borbély Y, Kern B, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013;258(5):690.
Spaniolas K, Trus TL, Adrales GL, et al. Early morbidity and mortality of laparoscopic sleeve gastrectomy and gastric bypass in the elderly: a NSQIP analysis. Surg Obes Relat Dis. 2014;10(4):584–8.
Sippey M, Kasten KR, Chapman WH, et al. 30-day readmissions after sleeve gastrectomy versus Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2016;12(5):991–6.
Tarantino I, Barresi L, Petridis I, Volpes R, Traina M, Gridelli B. Endoscopic treatment of biliary complications after liver transplantation. World J Gastroenterol. 2008;14(26).
Rogers CC, Alloway RR, Alexander JW, et al. Pharmacokinetics of mycophenolic acid, tacrolimus and sirolimus after gastric bypass surgery in end-stage renal disease and transplant patients: a pilot study. Clin Transplant. 2008;22(3):281–91.
Aminian A, Brethauer SA, Andalib A, et al. Individualized metabolic surgery score: procedure selection based on diabetes severity. Ann Surg. 2017;266(4):650–7.
Froylich D, Corcelles R, Daigle C, et al. Effect of Roux-en-Y gastric bypass and sleeve gastrectomy on nonalcoholic fatty liver disease: a comparative study. Surg Obes Relat Dis. 2016;12(1):127–31.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2016;26(2):429–42.
Chopra T, Zhao JJ, Alangaden G, et al. Preventing surgical site infections after bariatric surgery: value of perioperative antibiotic regimens. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):317–28.
Aminian A, Brethauer SA, Sharafkhah M, et al. Development of a sleeve gastrectomy risk calculator. Surg Obes Relat Dis. 2015;11(4):758–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
De-identified patient information is freely available to all institutional members who comply with the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) Data Use Agreement. The Data Use Agreement implements the protections afforded by the Health Insurance Portability and Accountability Act of 1996 and the ACS NSQIP Hospital Participation Agreement, and conforms to the Declaration of Helsinki.
Informed Consent
For this type of study on de-identified datasets, formal consent is not required.
ACS NSQIP Disclaimer
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Rights and permissions
About this article
Cite this article
Minhem, M.A., Sarkis, S.F., Safadi, B.Y. et al. Comparison of Early Morbidity and Mortality Between Sleeve Gastrectomy and Gastric Bypass in High-Risk Patients for Liver Disease: Analysis of American College of Surgeons National Surgical Quality Improvement Program. OBES SURG 28, 2844–2851 (2018). https://doi.org/10.1007/s11695-018-3259-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3259-z