Abstract
Background
This study aimed to assess quality of life in obese patients 1 year after bariatric surgery taking into consideration the influence of socio-demographic, clinical, and psychological variables.
Methods
A sample of 90 patients undergoing bariatric surgery was assessed in two moments: before surgery and 1 year after surgery.
Results
Social support, problem-focused coping strategies, and quality of life increased after surgery, while eating disorder behaviour and impulsiveness decreased. The presence of eating disorder behaviour predicted worse physical and mental quality of life and higher satisfaction with social support predicted better physical and mental quality of life. In addition, higher impulsiveness predicted worse mental quality of life. Spirituality moderated the relationship between impulsiveness and mental/physical quality of life.
Conclusions
Interventions should focus on promoting social support and coping strategies particularly spirituality since it played an important role in quality of life.
Similar content being viewed by others
Introduction
Obesity is defined by the World Health Organization (WHO) as abnormal or excessive fat accumulation (body mass index equal or higher than 30) that may impair health [1]. Obesity may be considered a chronic disease, but also a risk factor for the development of other chronic diseases associated with the highest rates of morbidity and mortality [2]. It is a problem of public health that already reached epidemic proportions [1, 2] with WHO data indicating that, in 2016, there were more than 1.9 billion adults with overweight and 650 million with obesity [1]. Overweight and obesity are still responsible for roughly 2.8 million deaths per year [1]. Portugal is no exception with more than half of the population, 5.9 million of people, being obese or pre-obese. The prevalence is higher in older adults, with eight in each ten being obese or pre-obese [3]. These facts illustrate the need to better understand obesity and psychological variables that may impair individuals’ QoL.
Bariatric surgery is being increasingly recommended to treat patients with severe or morbid obesity (body mass index—BMI > 40 kg/m2 and BMI > 35 kg/m2, respectively) that have not succeeded in losing weight through non-surgical methods [4]. This surgery is also described as the best option for weight loss in terms of long-term effects [5]. Still, its success depends on socio-demographic variables, such as age and gender [6]. Therefore, younger patients tend to lose more weight, mainly due to lower associated comorbidities and greater physical mobility [7]. Moreover, there is a tendency for obese individuals since childhood/adolescence to lose more weight after surgery than for those whose obesity onset only occurred in adulthood [8]. Regarding gender, female patients tend to suffer more from negative social effects and weight loss, which leads to worse mental QoL, while male patients appear to be more concerned with medical problems than with weight loss itself [9].
Obesity entails several problems for physical and mental health and, thus, directly and significantly affects QoL [10]. Patients with higher degrees of obesity reported worse QoL than those with lower degrees. Therefore, higher levels of obesity are associated with a decrease in QoL [11]. Bariatric surgery has been associated with a significant increase in health-related quality of life and physical QoL and is positively associated with a decrease in BMI [12]. This pattern of increased QoL after surgery often coincides with the phase of major weight loss, which generally takes place between 1 and 3 years after the surgery [13]. However, weight loss per se is not sufficient to explain the oscillations in QoL, after surgery. Other factors such as decreased medical comorbidities and maladaptive eating behaviors, as well as perceived social support, may contribute to this increase in QoL [14].
Eating disorder behaviors before the surgery may also persist after, leading to lower weight losses and poorer QoL [4] and playing an important role as a negative predictor of QoL, more evident on mental QoL [15, 16]. After surgery, eating disorders may develop as a compensatory behavior, such as inducing vomiting, to regulate weight loss and body image [17]. However, eating patterns may stabilize after surgery, decreasing eating disorder behavior present before the surgery [18]. For these reasons, it is sometimes difficult to predict which patients will progress positively over time [18].
Impulsiveness is the predisposition to react quickly and without planning to stimuli, not taking into account the negative consequences [19], and may also play a role in eating behavior, since impulsive individuals tend to eat uncontrollably more often, despite the fact that impulsiveness alone does not predict eating pathology [20]. Impulsiveness before bariatric surgery has been associated with the presence of eating disorders and is considered a positive predictor of post-surgery impulsiveness [21]. Higher impulsiveness assessed, at post-surgery, negatively predicted weight loss 1 year after surgery and was associated with higher rates of eating disorders and worse QoL [21].
Obese patients with a positive perception of social support tend to face the post-surgery treatment positively, since they feel supported. In fact, social support was found to be a mediator in the process of physical or mental health/illness [22] in obese patients and those with a positive perception of their social support showed a higher weight loss and better QoL [23]. Social support is considered crucial to cope with the several post-surgery psychosocial stressors and dietary changes [24]. Nevertheless, social support may also be a negative predictor of QoL since Canetti, Berry, and Elizur [25] found that patients who perceived more social support ingested more food in social events and, consequently, showed worse QoL.
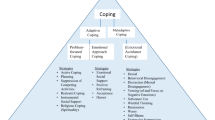
Obese patients who seek treatment often use emotion-focused coping strategies, which in turn are associated with greater distress, since patients may try to regulate their negative emotions with excessive food intake [26]. Problem-focused coping strategies, in turn (e.g., fighting spirit), are associated with less distress [27]. Individuals with emotion-focused coping show increased psychological distress, while problem-focused coping has been associated with improved mental health. Obese individuals report a greater use of emotion-focused coping strategies to deal with problems [28].
Spirituality has become increasingly important in chronic illness [29]. Patients with higher levels of spirituality, who attribute greater meaning to life, are less affected by negative emotional states, report greater well-being and better adjustment, as well as seeking out more social support, vital in post-surgery treatment [30]. Moreover, spirituality moderated the relationship between chronic illness and QoL [31, 32]. However, the role of spirituality as a moderator between impulsiveness and QoL, in post surgery, has not been analyzed.
Considering that the literature is not always consensual regarding the role of coping strategies, social support, and impulsiveness in obese patient’s Qol post-surgery, this study focused on QoL 1 year after bariatric surgery. It is expected that (1) social support, spirituality, and emotion- and problem-focused coping strategies will be positively associated with both physical and mental QoL, while eating disorder behavior and impulsiveness will not; (2) spirituality, social support, problem-focused coping, and physical and mental QoL will increase, whereas eating disorder behavior and impulsiveness will not, from the pre-surgery moment to the post-surgery moment; (3) use of more spirituality, less eating disorder behavior, more use of coping strategies lower impulsiveness, and high social support will predict better physical and mental QoL; (4) spirituality will moderate the relationship between impulsiveness and QoL, post-surgery.
Methods
Participants
The sample included 90 patients submitted to bariatric surgery in a major public hospital in North of Portugal, 1 year after surgery. Participants were 18 or older, with a pre-surgery BMI > 40 kg/m2, and cognitively able to answer questionnaires. Based on medical records, patients with a diagnosis of severe psychiatric disorders were excluded. There were 204 participants that underwent bariatric surgery. However, only 100 were in their first post-surgical year and were, therefore, invited to participate in the study. Only 90 participants were present the day of data collection.
Procedure
This study followed a prospective design with two assessment moments. Patients were identified and contacted by the psychologist of the Unit of Psychiatry and Mental Health. Patients were invited by letter and all signed an informed consent. Participation was voluntary. Patients answered the instruments in a room provided by the hospital for that purpose. The research protocol complied with the ethical principles contained in the Helsinki Declaration and was approved by the Hospital’s Ethics Committee.
Instruments
Clinical and Sociodemographic Questionnaire
Consists of 36 items that assess the individuals’ sociodemographic (gender, age, education, marital, and professional status) and clinical characteristics (weight, BMI, obesity onset, and physical activity practice). Patients’ weight considered was the last weight recorded in the patient’s chart before surgery.
Short Form Health Survey–SF 36 [33, 34]
The SF 36 assesses QoL through eight subscales: physical functioning (α = .93), physical role functioning (α = .82), bodily pain (α = .95), general health perceptions (α = .82), emotional role functioning (α = .83), social role functioning (α = .90), vitality (α = .82), and mental health (α = .80). Higher scores indicate better perceptions of health status. In the Portuguese validation [34], these subscales are grouped into two main domains: physical QoL and mental QoL. In this study, the Cronbach alpha for physical QoL was .93 and .95 for mental QoL. In the Portuguese version, only convergent validity was assessed with the Darthmouth Cooperative Functional Assessment Charts (COOP) that measures functional health and the correlations between the physical and mental dimensions of SF-36 and COOP ranged between .24 e .69 showing good convergent validity.
Barratt Impulsiveness Scale (BIS-11) [35, 36]
Comprises 30 items assessing attention, motor, and nonplanning impulsiveness. Higher results indicate higher impulsiveness. The original version showed a Cronbach alpha of .62 for the total scale, whereas in this study was .59. The Portuguese version presents good convergent validity (r = .307) with the Neuroticism Scale from Eysenck Personality Questionnaire- Revised (EPQ–R). The divergent validity was assessed with the Social Desirable Scale and EPQ–R (with r = .01 and r = − .30, respectively) showing good divergent validity.
Satisfaction with Social Support Scale [37]
Composed of 15 items that assess satisfaction with social support organized into four subscales: “satisfaction with friendships”, “intimacy”, “family satisfaction”, and “social activities”. Higher scores correspond with higher levels of satisfaction with social support. In this study, only the total scale was used, with a Cronbach alpha of .89 while in the original version was .85. The instrument presented good convergent validity with the Mental Health Inventory (r = .55) and the correlation between the item and the scales showed good discriminant validity.
Ways of Coping Questionnaire [38, 39]
Consists of 48 items and analyzes the strategies that the individual uses to deal with several specific situations of stress. The items are organized into eight subscales: confrontive coping, self-controlling, seeking social support, accepting responsibility, planful problem-solving, distancing, escape-avoidance, and positive reappraisal. These subscales are grouped into two dimensions: emotion-focused and problem-focused coping. Higher scores in each dimension indicate greater use of the respective coping strategies. The Cronbach alphas of the eight subscales ranged from .65 to .80. In this study, the Cronbach alphas were .86 for problem-focused coping and .71 for emotion-focused coping. The Portuguese version presents moderate convergent validity for emotion-focused coping dimension (.24 < r < .31) with all dimensions of the Zung Anxiety Scale, whereas the problem-focusing coping dimension did not show significant correlations, revealing good discriminant validity.
Spiritual and Religious Attitudes in Dealing with Illness (SpREUK) [40, 41]
This questionnaire consists of 15 items divided into three subscales: “search (for support/access)”, “trust (in a higher guidance/source)”, and “reflection (positive interpretation of the disease)”. The total scale was used in this study, with a Cronbach alpha of .93 while in the original version was of .94. Higher scores indicate higher levels of spirituality. The Portuguese version showed good convergent validity with the Revised Dyadic Adjustment scale (r = .125, p < .001).
Eating Disorder Examination-Questionnaire (EDE-Q) [42, 43]
The instrument includes 28 items that assess behavior, attitudes, and feelings associated with eating disorders. A global score of eating disorder behavior is the average score of the four subscales: “restraint”, “eating concern”, “shape concern”, and “weight concern”. Cronbach alpha for the total scale in the original study was .85 and in this study was .91. The Portuguese version used the ROC analysis to assess whether EDE-Q could discriminate if a participant presented or not an eating disorder. The ROC analysis showed that EDE-Q had a good discriminant power.
Data Analysis
Statistical analyses were made using version 22.0 of IBM’s SPSS® software for Windows. Parametric tests were used when the corollaries for their use were present. The presence of multicollinearity was also tested with the VIF (≤ 5) and tolerance value (> .20) [44]. The Pearson/Spearman correlation test was used to assess the relationship between continuous variables and the Point-Bisserial between continuous and categorical variables. In order to analyze differences between pre- and post-surgery, t tests for paired samples were used and MANOVA for repeated measures. A hierarchical regression (enter method) was performed to analyze predictors of QoL. The regression model only included variables associated with physical and/or mental QoL. Finally, a moderation analysis was performed using the macro command process version 2.16.1 for SPSS [45].
Results
Sample Characteristics
This study included 90 patients 1 year after bariatric surgery. Of the total sample, 87.8% were women aged 24 to 68 years old (M = 45.14, SD = 10.13). A gastric bypass was performed in 85.6% of participants and gastric sleeve in the remaining 14.4%. Regarding marital status, 22.2% were single, 67.8% were married, 6.7% were separated/divorced, and 3.3% were widowers. Ninety percent had no difficulties in following the recommended diet and 12% reported the habit of vomiting after meals. The mean BMI was 29.2 kg/m2 (SD = 3.89), which falls within the overweight category, ranging between 21.36 and 38.46 kg/m2. Specifically, 15.6% showed normal weight, 37.8% were overweight, 38.9% had moderate obesity, and 7.8% still fell within the severe obesity category. The mean percentage of weight lost was 33.86% (SD = 6.88%), and the mean percentage of excess weight lost was 80.83% (SD = 17.50%).
Relationship Between Sociodemographic, Clinical, and Psychological Variables
A negative association between mental QoL and eating disorder behavior (r = − .39, p < .001) and impulsiveness (r = − .62, p < .001) was found. There was also a significant negative association between physical QoL and eating disorder behavior (r = − .36, p < .001) and impulsiveness (r = − .42, p < .001). Thus, greater eating disorder behavior and impulsiveness were associated with worse mental and physical QoL. There was a significant positive association between mental QoL and social support (r = .71, p < .001) and physical QoL (r = .77, p < .001) and between physical QoL and social support (r = .53, p < .001). Therefore, better mental QoL was associated with better physical QoL, and higher levels of satisfaction with social support were associated with better mental and physical QoL. The Point-Bisserial correlation test revealed a significant positive association between marital status and social support (rpb = .23, p = .03), physical QoL (rpb = .23, p = .01), and mental QoL (rpb = .21, p = .04) and a negative association between marital status and spirituality (rpb = − .31, p = .01). The Spearman correlation test showed a significant positive association between the onset of obesity and eating disorder behavior (rs = .25, p = .02), and education level and problem-focused coping (rs = .21, p = .05), as well as a significant negative association between education level and spirituality (rs = − .40, p < .001), and eating disorder behavior (rs = − .23, p = .03). The Chi-square test revealed a significant positive association between gender and education level (χ2 = 12.54, p = .01) and between education level and the onset of obesity (χ2 = 16.32, p = .01), (Table 1).
Differences Between Pre- and Post-surgery on Psychological Variables
There were significant differences from pre-surgery to post-surgery on physical QoL (F = 208.42, p < .001, η2 = .70), mental QoL (F = 21.13, p < .001, η2 = .21), problem-focused coping (F = 33.93, p < .001, η2 = .276), eating disorder behavior (t = 2.25, p < .001, f2 = .29), and social support (t = − 8.68, p < .001, f2 = .92). After surgery, mental and physical QoL was higher, more problem-focused coping strategies were used, satisfaction with social support was higher, and the presence of eating disorders decreased (see Table 2).
Predictors of Mental and Physical QoL
The linear regression model was significant (F = 6.78, p < .001), explaining 31.3% of the variance of physical QoL. Eating disorder behavior negatively predicted physical QoL (β = − .20, t = − 2.09, p = .04), whereas satisfaction with social support positively predicted physical QoL (β = .34, t = 3.07, p = .01). Thus, the presence of eating disorder behavior predicted worse physical QoL and higher satisfaction with social support predicted better physical QoL.
The linear regression model was significant (F = 18.44, p = .001), explaining 57.8% of the variance of mental QoL. Eating disorder behavior (β = − .16, t = − 2.13, p = .04) and impulsiveness (β = − .33, t = − 3.88, p < .001) were negative predictors of mental QoL, while social support was a positive predictor (β = .510, t = 5.83, p < .001). Thus, the presence of eating disorder behavior and higher impulsiveness predicted worse mental QoL and higher satisfaction with social support predicted better QoL (see Table 3).
Post-surgery Spirituality as a Moderator of the Relationship Between Impulsiveness Before Surgery and QoL Post-Surgery
Spirituality after surgery moderated the relationship between pre-surgery impulsiveness and mental QoL post-surgery, i.e., the negative relationship between impulsiveness and mental QoL was stronger when post-surgery spirituality was lower (t = − 2.57, p = .01; see Fig. 1). Post-surgery spirituality also moderated the relationship between pre-surgery impulsiveness and physical QoL post-surgery, i.e., the negative relationship between impulsiveness and physical QoL was stronger when post-surgery spirituality was lower (t = − 2.04, p = .04; see Fig. 2).
Discussion
This study aimed to assess QoL in obese patients 1 year after bariatric surgery taking into consideration the influence of socio-demographic, clinical, and psychological variables.
Physical and mental QoL were positively associated with satisfaction with social support, indicating that individuals satisfied with their social support showed a positive perception of their QoL [23, 46]. The presence of eating disorder behavior and high impulsiveness were negatively associated with QoL, indicating that eating disorder behavior may interfere with several physical, emotional, and social aspects of the individual’s life [47]. Moreover, impulsive patients showed lower QoL, and this result makes intuitive sense since these patients may have difficulty accepting the dietary patterns after surgery [47], required to maintain less weight and, consequently, report worse QoL [48]. Eating disorder behavior was positively associated with impulsiveness and the literature reported that impulsiveness is considered a prominent factor in the onset of eating disorders [49]. Satisfaction with social support was negatively associated with emotion-focused coping, eating disorder behavior, and impulsiveness. In fact, patients who are more satisfied with their social support may adopt less emotion-focused coping strategies, since they have access to their support network to help them deal with their problems [50]. Additionally, more impulsive individuals tend to have smaller support networks and, consequently, perceive less social support [51] and may compensate social isolation with food, which may contribute to the development of eating disorder behavior [52]. Emotion-focused coping was positively associated with spirituality and eating disorder behavior. These results may be explained by the fact that spirituality is perceived as a coping strategy per se [53]. On the other hand, emotion-focused coping was associated with eating disorder behavior, and that result may indicate that food could be perceived as a strategy of emotional regulation [54].
Patients who were submitted to bariatric surgery showed high QoL, eating disorder behavior, satisfaction with social support, and problem-focused coping, 1 year after the surgery. Previous studies found that QoL increased significantly after bariatric surgery [55], particularly physical QoL, since it was associated with weight loss [12]. As expected, the presence of eating disorder behavior decreased. In fact, after surgery, eating patterns tend to stabilize and the physiological nature of the surgery also attenuates the compulsive food intake [14]. Satisfaction with social support and problem-focused coping were also higher, after surgery. Patients who succeed in losing weight perceive greater social support [24], and problem-focused coping strategies have been associated with better mental QoL [28]. Spirituality and impulsiveness did not differ between the two moments (pre and post-surgery), which may suggest that these variables are more related to personality traits and, therefore, less vulnerable to changes in short periods of time, such as 1 year [56]. Future studies should confirm these results with longer periods of assessment, after surgery.
Satisfaction with social support was a positive predictor of both physical and mental QoL. This result is congruent with the literature that shows social support as a positive predictor of health-related QoL [57]. In fact, perceived social support, both pre- and post-surgery, is important in weight loss and increased QoL [23]. Therefore, one may hypothesize that satisfaction with social support may also facilitate adherence to the new diet patterns, since patients’ perception of the received support may indicate approval from their social network predicting, as a result, better Qol. Future studies should also test the moderating role of adherence to diet between social support and QoL.
The presence of an eating disorder behavior was a negative predictor of both physical and mental QoL corroborating previous studies [15, 16]. Patients with eating disorder behavior, after surgery, tend to lose less weight when compared to patients without these disorders, suggesting that deregulated eating behaviors may persist after surgery and have a negative influence on QoL [58]. This result also may indicate that an eating disorder may be more associated with inadequate psychological patterns than eating needs. Moreover, impulsiveness was a negative predictor of mental QoL. Loss of control and high levels of impulsiveness after surgery have been negatively associated with BMI mental QoL [59]. However, this result needs to be interpreted with caution since impulsiveness was assessed as a general trait in life’s decisions and not specific to food choices. However, impulsiveness was not a predictor of physical QoL, indicating that the post-surgery physical improvements were not easily influenced by the subjective perception of loss of control [21].
In this study, work status did not predict QoL, probably due to the low number of participants that were employed. However, previous findings have shown that being employed is an important predictor of both physical and mental QoL [28]. Future studies with bigger samples need to test this result.
Post-surgery spirituality was a moderator between pre-surgery impulsiveness and post-surgery physical and mental QoL. The negative relationships was stronger when spirituality was lower showing that when impulsive individuals used less spirituality, as a coping mechanism, they reported worse QoL. Impulsive patients that reported better QoL were, those who used more often spirituality as a coping mechanism. Therefore, one may assume that patients between the pre- and post-surgery moments became more aware of their internal resources such as spirituality with a positive impact on their QoL. This result emphasizes the importance of spirituality as a coping mechanism, in obese patients. Spirituality may help patients face adversity in dealing with stressful events [60]. It would be important, in future studies, to assess and analyze whether locus of control also changed between the pre-post-surgery since that indicator may be associated with spirituality post-surgery.
Limitations
This study has some limitations that should be taken into account in future studies such as gender, since the majority were females, as well as the exclusive use of the self-report measures. In addition, this study only included two assessment moments and future studies, using a longitudinal design, should assess changes over longer periods of time in QoL and include adherence to lifestyle changes in both the patient and their partners.
Conclusion
According to the results, intervention in multidisciplinary teams should focus on support networks to increase QoL, while at the same time assess eating disorder behavior that may compromise treatment success. In addition, interventions with this population should include coping strategies, with particular attention to spirituality, since this variable was a moderator in the relationship between impulsiveness and QoL.
References
WHO.int [Internet]. 10 facts on obesity. Available from: http://www.who.int/features/factfiles/obesity/en/. Accessed October 2017.
Camolas J, Gregório MJ, Sousa SM, Graça P. Programa Nacional Para a Promoção da Alimentação Saudável. Obesidade: Otimização da Abordagem Terapêutica no Serviço Nacional de Saúde [National Program for the promotion of healthy food. Obesity: optimizing the therapeutic approach in the Nacional health service]. Lisboa: Direção-Geral da Saúde; 2017.
Lopes C, Torres D, Oliveira A, Severo M, Alarcão V, Guiomar S, et al. Inquérito Alimentar Nacional e de Atividade Física 2015–2016: Relatório Parte II [National Food and Physical Activity Survey 2015–2016: Report Part II]. Porto: Universidade do Porto; 2017
Parker K, Mitchell S, Brien O, et al. Psychometric evaluation of disordered eating measures in bariatric surgery patients. Eat Behav. 2015;19:39–48. https://doi.org/10.1016/j.eatbeh.2015.05.007.
Dimick J, Birkmeyer J. Rethinking eligibility criteria for bariatric surgery. JAMA. 2014;312:953–4. https://doi.org/10.1001/jama.2014.3836.
Averbukh Y, Heshka S, El-Shoreya H, et al. Depression scores predict weight loss following roux-en-Y gastric bypass. Obes Surg. 2003;13(6):833–6.
Busetto L, Segato G, De Marchi F, et al. Outcome predictors in morbidly obese recipients of an adjustable gastric band. Obes Surg. 2002;12(1):83–92.
Rowe J, Downey J, Faust M, et al. Psychological and demographic predictors of successful weight loss following silastic ring vertical stapled gastroplasty. Psychol Rep. 2000;86:1028–36. https://doi.org/10.2466/PR0.86.3.1028-1036.
Christiansen B, Borge L, Fagermoen S. Understanding everyday life of morbidly obese adults-habits and body image. Int J Qual Stud Health Well Being. 2012;7:1–9. https://doi.org/10.3402/qhw.v7i0.17255.
Costa R, Yamaguchi N, Santo M, et al. Outcomes on quality of life, weight loss, and comorbidities after roux-in-Y gastric bypass. Arq Gastroenterol. 2014;51:165–70. https://doi.org/10.1590/S0004-28032014000300002.
Brilmann M, Oliveira S, Thiers O. Avaliação da qualidade de Vida relacionada a saúde na obesidade [evaluation of health related quality of life in obesity]. Cad Saude Colet. 2007;15(1):39–54.
Alger-Mayer S, Malone M, Polimeni JM. Health related quality of life after gastric bypass surgery. Appl Res Qual Life. 2011;7:155–61.
Strain GW, Kolotkin RL, Dakin GF, et al. The effects of weight loss after bariatric surgery on health-related quality of life and depression. Nutr Diabetes. 2014;4:1–6. https://doi.org/10.1038/nutd.2014.29.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26:395–409. https://doi.org/10.1007/s11695-015-1940-z.
Brunault P, Frammery J, Couet C, et al. Predictors of changes in physical, psychosocial, sexual quality of life, and comfort with food after obesity surgery: a 12-month follow-up study. Qual Life Res. 2015;24:493–502. https://doi.org/10.1007/s11136-014-0775-8.
Colles S, Dixon J, O’Brien P. Grazing and loss of control related to eating: two high-risk factors following bariatric surgery. Obesity. 2008;16:615–22. https://doi.org/10.1038/oby.2007.101.
Kubik J, Gill R, Laffin M, et al. The impact of bariatric surgery on psychological health. J Obes. 2013;2013:1–5. https://doi.org/10.1155/2013/837989.
Van Hout G, Fortuin F, Pelle A, et al. Psychological functioning, personality, and body image following vertical banded gastroplasty. Obes Surg. 2008;18:115–20. https://doi.org/10.1007/s11695-007-9309-6.
Moeller G, Barratt S, Dougherty M, et al. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–93. https://doi.org/10.1176/appi.ajp.158.11.1783.
Meule A, Platte P. Facets of impulsivity interactively predict body fat and binge eating in young women. Appetite. 2015;87:352–7. https://doi.org/10.1016/j.appet.2015.01.003.
White M, Kalarchian M, Masheb R, et al. Loss of control over eating predicts outcomes in bariatric surgery: a prospective 24-month follow-up study. J Clin Psychiatry. 2010;71:175–84. https://doi.org/10.4088/JCP.08m04328blu.
Symister P, Friend R. The influence of social support and problematic support on optimism and depression in chronic illness: a prospective study evaluating self-esteem as a mediator. Health Psychol. 2003;22:123–9. https://doi.org/10.1037/0278-6133.22.2.123.
Livhits M, Mercado C, Yermilov I, et al. Is social support associated with greater weight loss after bariatric surgery?: a systematic review. Obes Rev. 2011;12:142–8. https://doi.org/10.1111/j.1467789X.2010.00720.x.
Henrickson H, Ashton K, Windover A, et al. Psychological considerations for bariatric surgery among older adults. Obes Surg. 2009;19:211–6. https://doi.org/10.1007/s11695-008-9768-4.
Canetti L, Berry E, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight-loss program: the mediating role of emotional eating. Int J Eat Disord. 2009;42:109–17. https://doi.org/10.1002/eat.20592.
Li W. Rukavina P. a review on coping mechanisms against obesity bias in physical activity/education settings. Obes Rev. 2009;10:87–95. https://doi.org/10.1111/j.1467-789X.2008.0.
Rydén A, Karlsson J, Sullivan M, et al. Coping and distress: what happens after intervention? A 2-year follow-up from the Swedish obese subjects (SOS) study. Psychosom Med. 2003;65:435–42. https://doi.org/10.1097/01.PSY.0000041621.25388.1A.
Lerdal A, Andenæs R, Bjørnsborg E, et al. Personal factors associated with health-related quality of life in persons with morbid obesity on treatment waiting lists in Norway. Qual Life Res. 2011;20:1187–96. https://doi.org/10.1007/s11136-011-9865-z.
Adegbola M. Spirituality and quality of life in chronic illness. J Theory Constr Test. 2006;10(2):42–6.
Heather H, Kathleen A, Windover A, et al. Psychological considerations for bariatric surgery among older adults: a review. Obes Surg. 2009;19:211–6. https://doi.org/10.1007/s11695-008-9768-4.
Pirutinsky S, Rosmarin D, Holt C. Religious coping moderates the relationship between emotional functioning and obesity. Health Psychol. 2012;31:394–297. https://doi.org/10.1037/a0026665.
Miller W, Thoresen E. Spirituality, religion, and health: an emerging research field. Am Psychol. 2003;58:24–35. https://doi.org/10.1037/0003-066X.58.1.24.
Ware JE, Snow KK, Kosinski M, et al. SF-36 health survey manual and interpretation guide. Boston: New England Medical Center; 1993.
Ferreira PL. Criação da versão Portuguesa do MOS SF36. Parte I – Adaptação Cultural e Linguística [Development of the Portuguese version of MOS SF-36. Part I. Cultural and linguistic adaptation]. Acta Medica Port. 2000;13(1–2):55–66.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74.
Diemen L, Szobot C, Kessler F, et al. Adaptation and construct validation of the Barratt impulsiveness scale (BIS 11) to Brazilian Portuguese for use in adolescents. Rev Bras Psiquiatr. 2006;29:153–6. https://doi.org/10.1007/s10826-016.0453.2.
Pais-Ribeiro JL. Escala de Satisfação com o Suporte social (ESSS) [satisfaction scale with social support (SSSS)]. Análise. Psicológica. 1999;3(17):547–58.
Folkman S, Lazarus RS. Manual for the ways of coping questionnaire (research edition). California: Consulting Psychologists Press; 1988.
Pais-Ribeiro J, Santos C. Estudo conservador de adaptação do ways of coping questionnaire a uma amostra e contexto Portugueses [conservative study of adaptation of the ways of coping questionnaire to a Portuguese sample and context]. Análise. Psicológica. 2001;4(19):491–502.
Ostermann T, Bussing A, Matthiessen P. Role of religion and spirituality in medical patients: confirmatory results with the SpREUK questionnaire. Health Qual Life Outcomes. 2005;3:3–10. https://doi.org/10.1186/1477-7525-3-10.
Pereira MG, Pedras S, Bacalhau R, Santos D. Research Group in Family Health & Illness. Psychometric properties of Spreuk in Women with HPV and Cancer. Unpublished Manuscript. 2018.
Fairburn G, Beglin J. Assessment of eating disorders: interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–70. https://doi.org/10.1002/1098-108.
Machado P. Versão Portuguesa do EDE-Q [Portuguese version of the EDE-Q]. unpublished manuscript. Escola de Psicologia. Universidade do Minho. 2007.
Field A. Discovering statistics using SPSS. 3rd ed. London: Sage; 2009.
Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: Guilford Press; 2013.
Bravo J, Mandich C, Castrillón F, et al. Cirugía bariátrica en adultos: Facilitadores y obstaculizadores de la pérdida de peso desde la perspectiva de los pacientes [Bariatric surgery in adults: Variables that facilitate and hinder weight loss from pacients perspective]. Nutr Hosp. 2015;3:1504–12. https://doi.org/10.3305/nh.2015.31.4.8515.
Costa J, Pinto S. Transtorno da compulsão alimentar periódica e Qualidade de Vida de pacientes candidatos a cirurgia bariátrica [binge eating disorder and quality of life of candidates to bariatric surgery]. Arq Bras Cir Dig. 2015;28(1) https://doi.org/10.1590/S01026720201500S100015.
Kroes M, Osei-Assibey G, Baker-Searle R, et al. Impact of weight change on quality of life in adults with overweight/obesity in the United States: A systematic review. Curr Med Res Opin. 2016;32:485–508. https://doi.org/10.1185/03007995.2015.1128403.
Annagür BB, Orhan O, Özer A, et al. The effects of depression and impulsivity on obesity and binge eating disorder. Klinik Psikofarmakol Bülteni. 2015;25:162–70. https://doi.org/10.5455/bcp.20130408021434.
Hugh R, Feeters D, Boyda D, et al. Coping styles in adults with cystic fibrosis: implications for emotional and social quality of life. Psychol Health Med. 2015;21:102–12. https://doi.org/10.1080/13548506.2015.1020317.
Coco L, Gullo S, Salerno L, et al. The association among interpersonal problems, binge behaviors, and self-esteem, in the assessment of obese individuals. Compr Psychiatry. 2011;52:164–70. https://doi.org/10.1016/j.2010.06.002.
Schwartz TL, Nihalani N, Jindal S, et al. Psychiatric medication induced obesity: a review. Obes Rev. 2004;5:115–21. https://doi.org/10.1111/j.1467-789X.2004.00139.x.
Ano G, Vasconcelles E. Religious coping and psychological adjustment to stress: a meta-analysis. J Clin Psychol. 2005;61:461–80. https://doi.org/10.1002/jclp.20049.
Matera A, Schiltz L. Comparative structural study of the configuration of coping strategies among female patients with eating disorders and non-clinical control group. Psychiatr Danub. 2013;25(4):359–65.
Julia C, Ciangura C, Capuron L, et al. Quality of life after roux-en-y gastric bypass and changes in body mass index and obesity-related comorbidities. Diabetes Metab. 2013;39:148–54. https://doi.org/10.1016/j.diabet.2012.10.008.
de Maria C, Yaegashi S. The traits personality associated with the development of obesity. Rev Bras Obes, Nutr Emagrecimento. 2016;10(56):74–92.
Sabbioni ME, Dickson MH, Eychmüller S, et al. Intermediate results of health related quality of life after vertical banded gastroplasty. IJO. 2002;26:277–80. https://doi.org/10.1038/sj/ijo/0801879.
Zwaan M, Mitchel JE. Eating disorders and eating behavior pre- and post-bariatric surgery. In: Still C, Sarwer D, Blankenship J, editors. The ASMBS textbook of bariatric surgery. New York: Springer; 2014. https://doi.org/10.1007/978-1-4939-1197-4_42014.
Tambelli R, Cerniglia L, Cimino S, et al. An exploratory study on the influence of psychopathological risk and impulsivity on BMI and perceived quality of life in obese patients. Nutrients. 2017;9:431. https://doi.org/10.3390/nu9050431.
Pargament KI, Abu Raiya H. A decade of research on the psychology of religion and coping: things we assumed and lessons we learned. Psyke & Logos. 2007.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study followed a prospective design with two assessment moments. Patients were identified and contacted by the psychologist of the Unit of Psychiatry and Mental Health. Patients were invited by letter and all signed an informed consent. Participation was voluntary. Patients answered the instruments in a room provided by the hospital for that purpose. The research protocol complied with the ethical principles contained in the Helsinki Declaration and was approved by the Hospital’s Ethics Committee.
Conflict of Interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pereira, M.G., Faria, S. & Lopes, H. Quality of Life One Year After Bariatric Surgery: the Moderator Role of Spirituality. OBES SURG 29, 1207–1215 (2019). https://doi.org/10.1007/s11695-018-03669-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-03669-4