Abstract
Background
In obese patients (OP), the best intraoperative ventilation strategy remains to be defined. Dynamic lung compliance (Cdyn) and dead space fraction are indicators of efficient ventilation at an optimal positive end-expiratory pressure (PEEP). Herein, we investigated whether intraoperative dynamic lung compliance optimization through PEEP manipulations affects the incidence of postoperative hypoxemia (SpO2 < 90%) in OP undergoing laparoscopic bariatric surgery (LBS).
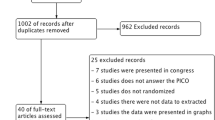
Methods
This was a single-center, prospective, randomized controlled study conducted from July 2013 to December 2015. After obtaining institutional review board approval and informed consent, 100 OP undergoing LBS under volume-controlled ventilation (tidal volume 8 mL/kg of ideal body weight) were randomized according to the PEEP level maintained during the surgery. In the control group, a PEEP of 10 cm H2O was maintained, while in the intervention group, the PEEP was adapted to achieve the best dynamic lung compliance. Anesthesia and analgesia were standardized. The patients received supplemental nasal oxygen on the first postoperative day and were monitored up to the second postoperative day with a portable pulse oximeter.
Results
Demographics were similar between groups. There was no difference in the incidence of hypoxemia during the first 2 postoperative days (control: 1.3%; intervention: 2.1%; p = 0.264).
Conclusions
The incidence of postoperative hypoxemia was not reduced by an open-lung approach with protective ventilation strategy in obese patients undergoing LBS. A pragmatic application of a PEEP level of 10 cm H2O was comparable to individual PEEP titration in these patients.
Trial Registration
Clinicaltrials.gov identifier, NCT02579798; https://clinicaltrials.gov/ct2/show/NCT02579798


Similar content being viewed by others
Data Availability
Data are available upon reasonable request to the corresponding author.
References
Coussa M, Proietti S, Schnyder P, et al. Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg. 2004;98(5):1491–5.
Magnusson L, Spahn DR. New concepts of atelectasis during general anaesthesia. Br J Anaesth. 2003;91(1):61–72.
Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology. 2005;102(4):838–54.
Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87(3):654–60.
Eichenberger A, Proietti S, Wicky S, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg. 2002;95(6):1788–92. table of contents
Imberger G, McIlroy D, Pace NL, et al. Positive end-expiratory pressure (PEEP) during anaesthesia for the prevention of mortality and postoperative pulmonary complications. Cochrane Database Syst Rev. 2010;9:56–67. https://doi.org/10.1002/14651858.CD007922.
Fernandez-Bustamante A, Hashimoto S, Serpa Neto A, et al. Perioperative lung protective ventilation in obese patients. BMC Anesthesiol. 2015;15(1):56.
Shander A, Fleisher LA, Barie PS, et al. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Crit Care Med. 2011;39(9):2163–72.
Futier E, Constantin J-M, Pelosi P, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;113(6):1310–9.
Whalen FX, Gajic O, Thompson GB, et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth Analg. 2006;102(1):298–305.
Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg. 2009;109(5):1511–6.
Almarakbi WA, Fawzi HM, Alhashemi JA. Effects of four intraoperative ventilatory strategies on respiratory compliance and gas exchange during laparoscopic gastric banding in obese patients. Br J Anaesth. 2009;102(6):862–8.
Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009;111(5):979–87.
Pelosi P, Ravagnan I, Giurati G, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91(5):1221–31.
Hemmes SN, Gama de Abreu M, Pelosi P, et al. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384(9942):495–503.
Tusman G, Böhm SH, Suarez-Sipmann F, et al. Alveolar recruitment improves ventilatory efficiency of the lungs during anesthesia. Can J Anesth. 2004;51(7):723–7.
Maracajá-Neto LF, Verçosa N, Roncally AC, et al. Beneficial effects of high positive end-expiratory pressure in lung respiratory mechanics during laparoscopic surgery. Acta Anaesthesiol Scand. 2009;53(2):210–7.
Meininger D, Byhahn C, Mierdl S, et al. Positive end-expiratory pressure improves arterial oxygenation during prolonged pneumoperitoneum. Acta Anaesthesiol Scand. 2005;49(6):778–83.
Futier E, Constantin JM, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–37.
Aldenkortt M, Lysakowski C, Elia N, et al. Ventilation strategies in obese patients undergoing surgery: a quantitative systematic review and meta-analysis. Br J Anaesth. 2012;109(4):493–502.
Gattinoni L, Carlesso E, Caironi P. Stress and strain within the lung. Curr Opin Crit Care. 2012;18(1):42–7.
Suter PM, Fairley B, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292(6):284–9.
Maisch S, Reissmann H, Fuellekrug B, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106(1):175–81.
Blankman P, Hasan D, Groot Jebbink E, et al. Detection of “best” positive end-expiratory pressure derived from electrical impedance tomography parameters during a decremental positive end-expiratory pressure trial. Crit Care. 2014;18(3):R95.
Carvalho ARS, Jandre FC, Pino AV, et al. Effects of descending positive end-expiratory pressure on lung mechanics and aeration in healthy anaesthetized piglets. Crit Care. 2006;10(4):R122.
Terragni PP, Rosboch G, Tealdi A, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;175(2):160–6.
Defresne AA, Hans GA, Goffin PJ, et al. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: a randomized controlled study. Br J Anaesth. 2014;113(3):501–7.
Severgnini P, Selmo G, Lanza C, et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118(6):1307–21.
Pelosi P, Gama de Abreu M, Rocco PR. New and conventional strategies for lung recruitment in acute respiratory distress syndrome. Crit Care. 2010;14(2):210.
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial I, Cavalcanti AB, Suzumura ÉA, et al. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318(14):1335–45.
Jo YY, Kwak HJ. What is the proper ventilation strategy during laparoscopic surgery? Korean J Anesthesiol. 2017;70(6):596–600.
Bluth T, Teichmann R, Kiss T, et al. Protective intraoperative ventilation with higher versus lower levels of positive end-expiratory pressure in obese patients (PROBESE): study protocol for a randomized controlled trial. Trials. 2017;18(1):202.
Acknowledgements
Assistance with the study: The authors would like to thank the following persons from the Department of Anaesthesiology, CHU Brugmann-HUDERF, Brussels, Belgium, who kindly performed the protocol study in the operating room: Ida Stany M.D., Robert Tircoveanu M.D., Yannick Ciccarella M.D., Jean-Louis Majcher M.D., Christiane Dzechi M.D., and Muj Mulaj M.D.
Funding
This work was supported only by CHU Brugmann-HUDERF departmental sources and the Brugmann foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Our study was a prospective, randomized controlled study, approved by the Institutional Ethics Committee. Written informed consent was obtained from all participating subjects. This manuscript adheres to the applicable Enhancing the Quality and Transparency of Health Research (EQUATOR) guidelines.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Ethical and Consent Statement
Ethical and consent statement provided by the Institutional Ethics Committee. Written informed consent was obtained from all participating subjects.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Annex 1: anesthetic protocol
Annex 1: anesthetic protocol
All subjects stopped consuming solid food from 6 h and clear liquids from 2 h before the elective surgery, and received 0.5–1 mg alprazolam and 150 mg ranitidine perorally, 1 h before the procedure as premedication.
Before induction, each patient was placed in ‘Ramp’ position. Basic monitoring was undertaken, including: electrocardiogram, non-invasive blood pressure (NIBP), and pulse oximetry oxygen saturation (SpO2).
An 18-gauge catheter was placed in a vein and a 20-gauge catheter in a radial artery. Further monitoring included entropy, thumb’s adductor neuromuscular monitor, nasopharyngeal temperature probe, and urinary catheter.
Anesthesia was induced by intravenous administration of propofol (2–3 mg/kg IBW) and sufentanil (GEPS model with target concentration of 0.3 ng/mL based on IBW: discontinued 1 h before the end of surgery). The intubation (tube size 8 for women and 8.5 for men) was facilitated by the administration of intravenous rocuronium (0.6 mg/kg corrected IBW). Antibiotic prophylaxis (cefazolin 2 g and metronidazole 500 mg) was also given at the induction.
Anesthesia was maintained with desflurane (6–8%) to keep entropy values between 40 and 60. Every 30 min, a train of 4 (TOF 50 Hz) was performed and a rocuronium bolus (0.15 mg/kg IBW) was administered as needed to maintain a TOF ratio of 0:4.
At the end of surgery, all patients received paracetamol (1 g). Neuromuscular blockade was checked at the thumb’s adductor. The neuromuscular blockade was reversed with 4 mg/kg (corrected IBW) sugammadex when the train-of-four (TOF) ratio reached 2:4.
After attaining a TOF ratio of 4:4 with a sustained tetanic stimulation at 100 Hz over 5 s, patients were placed in ‘Ramp’ position and the administration of desflurane and mechanical ventilation with volume control mode was discontinued in order to switch to mechanical ventilation with pressure support [PEEP of 5 cm H2O and 100% inspired fraction of oxygen (FiO2)].
Anti-emetic prophylaxis was administered to all patients as follows: 40 mg methylprednisolone at the induction and 4 mg ondansetron at the end of the intervention.
Thromboprophylaxis included intermittent pneumatic compression device beginning before surgery and low molecular weight heparin (80 mg/day) beginning 6 h after the procedure.
In the postoperative period, each patient received paracetamol 1 g every 6 h and patient-controlled intravenous analgesia with piritramide was started at the post-anesthesia care unit (PACU) (2-mg bolus every 7 min with a maximum of 30 mg in 4 h).
Rights and permissions
About this article
Cite this article
Van Hecke, D., Bidgoli, J.S. & Van der Linden, P. Does Lung Compliance Optimization Through PEEP Manipulations Reduce the Incidence of Postoperative Hypoxemia in Laparoscopic Bariatric Surgery? A Randomized Trial. OBES SURG 29, 1268–1275 (2019). https://doi.org/10.1007/s11695-018-03662-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-03662-x