Abstract
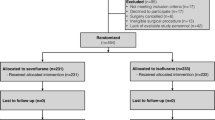
Early and clear recovery from anesthesia is the crux for preventing perioperative complications in the obese undergoing bariatric surgery. Volatile inhalation agents by virtue of high lipid solubility are expected to produce residual anesthetic effects. Prospective randomized trials comparing desflurane and sevoflurane used for anesthesia maintenance (electroencephalograph guided) during bariatric surgery published till 1st of July 2017 were searched in the medical database. Comparisons were made for surrogate markers of recovery from anesthesia that included time to eye-opening (TEo), time to tracheal-extubation (TEx), and Aldrete scores on immediately shifting to recovery (Ald-I). Five trials were included in the final analysis. Patients receiving desflurane began to respond faster by opening eyes on command (five trials) by 3.80 min (95%CI being 1.83–5.76) (random effects, P < 0.01, I2 = 78.61%), and tracheal extubation was also performed earlier (four trials) by 4.97 min (95%CI being 1.34–8.59). This meant a reduction of 37% in TEo and 33.60% in TEx over sevoflurane. Ald-I scores were higher/better with desflurane by 0.52 (95%CI being 0.19–0.84) (Fixed-effects, P < 0.01, I2 = 6.67%). Publication bias is likely for TEo (Egger’s Test, X-intercept = − 8.57, P = 0.02). No airway-related complications were reported with desflurane’s expedited recovery. Use of desflurane compared to sevoflurane for maintenance of anesthesia in morbidly obese patients allows attaining verbal contact faster, and tracheal extubating can be performed earlier without compromising safety. The benefits of better recovery extend into the immediate postoperative phase with patients being more awake upon shifting to the recovery.






Similar content being viewed by others
References
Singh PM, Panwar R, Borle A et al. Efficiency and safety effects of applying ERAS protocols to bariatric surgery: a systematic review with meta-analysis and trial sequential analysis of evidence. Obesity Surgery 2016; doi https://doi.org/10.1007/s11695-016-2442-3.
Thorell A, MacCormick AD, Awad S et al. Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 2016; doi https://doi.org/10.1007/s00268-016-3492-3.
Singh PM, Panwar R, Borle A, Mulier JP, Sinha A, Goudra B. Perioperative analgesic profile of dexmedetomidine infusions in morbidly obese undergoing bariatric surgery: a meta-analysis and trial sequential analysis. Surgery for Obesity and Related Diseases: Official Journal of the American Society for Bariatric Surgery 2017; doi https://doi.org/10.1016/j.soard.2017.02.025.
Alvarez A, Goudra BG, Singh PM. Enhanced recovery after bariatric surgery. Curr Opin Anaesthesiol. 2017;30:133–9.
Sinha AC, Singh PM. Controversies in perioperative anesthetic management of the morbidly obese: I am a surgeon, why should I care? Obes Surg. 2015;25:879–87.
Salihoglu Z, Karaca S, Kose Y, et al. Total intravenous anesthesia versus single breath technique and anesthesia maintenance with sevoflurane for bariatric operations. Obes Surg. 2001;11:496–501.
Esper T, Wehner M, Meinecke C-D, et al. Blood/gas partition coefficients for isoflurane, sevoflurane, and desflurane in a clinically relevant patient population. Anesth Analg. 2015;120:45–50.
Higgins JP, Green S. Guide to the contents of a Cochrane protocol and review. In: Fellow JPHSSV, Director SGF, editors. Cochrane handbook for systematic reviews of interventions. Ltd: John Wiley & Sons; 2008. p. 51–79.
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015;4:1.
Higgins JP, Altman DG. Assessing risk of bias in included studies. In: Fellow JPHSSV, Director SGF, editors. Cochrane handbook for systematic reviews of interventions. Ltd: John Wiley & Sons; 2008. p. 187–241.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
De Baerdemaeker LEC, Jacobs S, Den Blauwen NMM, et al. Postoperative results after desflurane or sevoflurane combined with remifentanil in morbidly obese patients. Obes Surg. 2006;16:728–33.
Ozdogan HK, Cetinkunar S, Karateke F, et al. The effects of sevoflurane and desflurane on the hemodynamics and respiratory functions in laparoscopic sleeve gastrectomy. J Clin Anesth. 2016;35:441–5.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Singh PM, Arora S, Borle A, et al. Evaluation of etomidate for seizure duration in electroconvulsive therapy: a systematic review and meta-analysis. The Journal of ECT. 2015;31:213–25.
Thiessen Philbrook H, Barrowman N, Garg AX. Imputing variance estimates do not alter the conclusions of a meta-analysis with continuous outcomes: a case study of changes in renal function after living kidney donation. J Clin Epidemiol. 2007;60:228–40.
Chowdhry AK, Dworkin RH, McDermott MP. Meta-analysis with missing study-level sample variance data. Stat Med. 2016;35:3021–32.
Lundh A, Gøtzsche PC. Recommendations by Cochrane review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. 2008;8:1–9.
Arain SR, Barth CD, Shankar H, et al. Choice of volatile anesthetic for the morbidly obese patient: sevoflurane or desflurane. J Clin Anesth. 2005;17:413–9.
Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22:233–6.
de Raaff CAL, Gorter-Stam MAW, de Vries N et al. Perioperative management of obstructive sleep apnea in bariatric surgery: a consensus guideline. Surg Obes Relat Dis: Off J Am Soc Bariatric Surg 2017; doi https://doi.org/10.1016/j.soard.2017.03.022.
Macario A, Dexter F, Lubarsky D. Meta-analysis of trials comparing postoperative recovery after anesthesia with sevoflurane or desflurane. American Journal of health-system pharmacy: AJHP: Official Journal of the American Society of Health-System Pharmacists. 2005;62:63–8.
Singh PM, Borle A, Shah D et al. Optimizing prophylactic CPAP in patients without obstructive sleep apnoea for high-risk abdominal surgeries: a meta-regression analysis. Lung2016 Feb 19; doi https://doi.org/10.1007/s00408-016-9855-6.
Boucher BA, Witt WO, Foster TS. The postoperative adverse effects of inhalational anesthetics. Heart Lung: J Crit Care. 1986;15:63–9.
Wadhwa A, Singh PM, Sinha AC. Airway management in patients with morbid obesity. Int Anesthesiol Clin. 2013;51:26–40.
Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011;74:1238–47.
Vallejo MC, Sah N, Phelps AL, et al. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth. 2007;19:3–8.
Kaur A, Jain AK, Sehgal R, et al. Hemodynamics and early recovery characteristics of desflurane versus sevoflurane in bariatric surgery. J Anaesthesiol Clin Pharmacol. 2013;29:36–40.
La Colla L, Albertin A, La Colla G, et al. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth. 2007;99:353–8.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
Not applicable.
Electronic supplementary material
ESM 1
Aldrete Scoring used in the studies to quantify recovery parameters. (DOCX 13 kb)
Rights and permissions
About this article
Cite this article
Singh, P.M., Borle, A., McGavin, J. et al. Comparison of the Recovery Profile between Desflurane and Sevoflurane in Patients Undergoing Bariatric Surgery—a Meta-Analysis of Randomized Controlled Trials. OBES SURG 27, 3031–3039 (2017). https://doi.org/10.1007/s11695-017-2929-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2929-6