Abstract
Introduction
Bariatric surgery patients are at high risk for venous thromboembolism (VTE), and chemoprophylaxis is recommended.
Methods
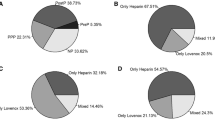
Sheikh Khalifa Medical City (SKMC) is an American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) member since 2009. We report the rates of VTE in bariatric surgery patients from 2010 to 2016 compared to ACS NSQIP bariatric surgery programs before and after switching from heparin to low molecular weight heparin (LMWH), initiating mandatory risk assessment using Caprini scoring for VTE and adopting an aggressive strategy for high-risk patients regarding dosage of LMWH and chemoprophylaxis after discharge.
Results
During the study period, there were 1152 cases (laparoscopic Roux-en-Y gastric bypass (LRYGB) 625 and laparoscopic sleeve gastrectomy (LSG) 527) at Bariatric & Metabolic Institute (BMI) Abu Dhabi compared to 65,693 cases (LRYGB 32,130 and LSG 33,563) at ACS NSQIP bariatric surgery programs. VTE rates remained stable at ACS NSQIP bariatric surgery programs from 2010 to 2016 (0.45, 0.45, 0.45, 0.25, 0.35, 0.3, and 0.3%). In contrast, VTE rates at BMI Abu Dhabi decreased from 2.2% in 2011 to 0.35% after we adopted an aggressive strategy to VTE without an increase in bleeding complications. LRYGB patients with VTE had higher OR time, leak, collection, and mortality at ACS NSQIP hospitals compared to those at BMI Abu Dhabi. In contrast, rates were similar in LSG patients with VTE.
Conclusion
Changing our approach to VTE management led our VTE rates to decrease and become like those of ACS NSQIP bariatric surgery patients in LSG and LRYGB.

Similar content being viewed by others
References
American Society for Metabolic and Bariatric Surgery Clinical Issues Committee ASMBS updated position statement on prophylactic measures to reduce the risk of venous thromboembolism in bariatric surgery patients. Surg Obes Relat Dis. 2013 Jul-Aug;9(4):493–7. doi: https://doi.org/10.1016/j.soard.2013.03.006.
Winegar DA, Sherif B, Pate V, et al. Venous thromboembolism after bariatric surgery performed by Bariatric Surgery Center of Excellence Participants: analysis of the bariatric outcomes longitudinal database. Surg Obes Relat Dis. 2011;7:181–8.
Becattini C, Agnelli G, Manina G, et al. Venous thromboembolism after laparoscopic bariatric surgery for morbid obesity: clinical burden and prevention. Surg Obes Relat Dis. 2012;8:108–15.
Finks JF, English WJ, Carlin AM, et al. Predicting risk for venous thromboembolism with bariatric surgery: results from the Michigan Bariatric Surgery Collaborative. Ann Surg. 255:1100–4.
Aminian A, Andalib A, Khorgami Z, et al. Who should get extended thromboprophylaxis after bariatric surgery?: a risk assessment tool to guide indications for post-discharge pharmacoprophylaxis. Ann Surg. 2017 Jan;265(1):143–50. https://doi.org/10.1097/SLA.0000000000001686.
Nimeri AA, Gamaleldin MM, McKenna KL, Turrin NP, Mustafa BO. Reduction of venous thromboembolism in surgical patients using a mandatory risk-scoring system: 5-year follow-up of an American College of Surgeons National Surgical Quality Improvement Program. Clin Appl Thromb Hemost. 2015 Nov 25. pii:
(ACS NSQIP Operational Manual 2015 chapter 4 page 123) www.acsnsqip.org
Nimeri A, Mohamed A, El Hassan E, et al. Are results of bariatric surgery different in the Middle East? Early experience of an international bariatric surgery program and an ACS NSQIP outcomes comparison. J Am Coll Surg. 2013;216(6):1082–8. https://doi.org/10.1016/j.jamcollsurg.2013.01.063.
Birkmeyer NJO, Finks JF, Carlin AM, et al. Comparative effectiveness of unfractionated and low-molecular-weight heparin for prevention of venous thromboembolism following bariatric surgery. Arch Surg. 2012;147(11):994–8.
Pannucci CJ, Shanks A, Moote MJ, et al. Identifying patients at high risk for venous thromboembolism requiring treatment after outpatient surgery. Ann Surg. 2012;255:1093–9.
Gupta PK, Franck C, Miller WJ, et al. Development and validation of a bariatric surgery morbidity risk calculator using the prospective, multicenter NSQIP dataset. J Am Coll Surg. 2011;212:301–9.
Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70–8.
Pannucci CJ, Laird S, Dimick JB, et al. A validated risk model to predict 90- day VTE events in postsurgical patients. Chest. 2014;145:567–73.
Scarborough JE, Cox MW, Mureebe L, et al. A novel scoring system for predicting postoperative venous thromboembolic complications in patients after open aortic surgery. J Am Coll Surg. 2012;214:620–6. discussion 627-8
Merkow RP, Bilimoria KY, McCarter MD, et al. Post-discharge venous thromboembolism after cancer surgery: extending the case for extended prophylaxis. Ann Surg. 2011;254:131–7.
Borkgren-Okonek MJ, Hart RW, Pantano JE, et al. Enoxaparin thromboprophylaxis in gastric bypass patients: extended duration, dose stratification, and antifactor Xa activity. Surg Obes Relat Dis. 2008;4:625–31.
Nutescu EA, Spinler SA, Wittkowsky A, et al. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009;43:1064–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
This article does not contain any studies with human participants or animals performed by any of the authors. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Nimeri, A.A., Bautista, J., Ibrahim, M. et al. Mandatory Risk Assessment Reduces Venous Thromboembolism in Bariatric Surgery Patients. OBES SURG 28, 541–547 (2018). https://doi.org/10.1007/s11695-017-2909-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2909-x