Abstract
Background and Aim
Even though health-related quality of life (HRQOL) is considered an important component of bariatric surgery outcome, there is a lack of HRQOL measures relevant for preoperative and postoperative patients. The objective of the current study was to develop a new instrument assessing HRQOL prior to and following bariatric surgery, entitled Quality of Life for Obesity Surgery (QOLOS) Questionnaire.
Methods
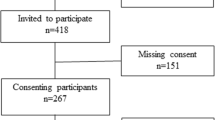
Topics for the QOLOS were initially generated via open-ended interviews and focus groups with 19 postoperative bariatric surgery patients. Qualitative analysis resulted in 250 items, which were rated by patients (n = 101) and experts (n = 69) in terms of their importance. A total of 120 items were retained for further evaluation and administered to 220 preoperative patients and 219 postoperative patients. They also completed a battery of other assessments to analyze issues of construct validity.
Results
Analyses resulted in a 36-item section 1 QOLOS form targeting both preoperative and postoperative aspects across seven domains (eating disturbances, physical functioning, body satisfaction, family support, social discrimination, positive activities, partnership) and a 20-item section 2 QOLOS form focusing on postoperative concerns only (domains: excess skin, eating adjustment, dumping, satisfaction with surgery). Subscales of both sections showed acceptable to excellent internal consistency (Cronbach’s α 0.72 to 0.95) and good convergent and discriminant validity.
Conclusion
The QOLOS represents a reliable and valid instrument to assess HRQOL in preoperative and postoperative patients. Future studies should test the questionnaire in larger samples consisting of patients undergoing different types of surgery.
Similar content being viewed by others
References
Bullinger M, Quitmann J. Quality of life as patient-reported outcomes: principles of assessment. Dialogues Clin Neurosci. 2014;16(2):137–45.
FDA. Guidance for industry. Patient-reported outcome measures: use in medical product development to suport labeling claims. 2009 [December 16, 2016]; Available from: http://www.fda.gov/downloads/Drugs/Guidances/UCM193282.pdf.
Raaijmakers LC, Pouwels S, Thomassen SE, et al. Quality of life and bariatric surgery: a systematic review of short- and long-term results and comparison with community norms. Eur J Clin Nutr. 2017;71(4):441–9.
Andersen JR, Aasprang A, Karlsen TI, et al. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis. 2015;11(2):466–73.
Sarwer DB, Lavery M, Spitzer JC. A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg. 2012;22(4):668–76.
Alvares RS, Beleigoli AM, Cancado AG, et al. Quality of life and weight loss in the long term after gastric bypass. Obes Surg. 2017;27(4):1069–70.
Reynolds CL, Byrne SM, Hamdorf JM. Treatment success: investigating clinically significant change in quality of life following bariatric surgery. Obes Surg. 2017;27(7):1842–8.
Peterhänsel C, Nagl M, Wagner B, et al. Predictors of changes in health-related quality of life 6 and 12 months after a bariatric procedure. Obes Surg. 2017;27(8):2120–8.
Biter LU, van Buuren MMA, Mannaerts GHH, Apers JA, Dunkelgrun M, Vijgen G, 2017. Quality of life 1 year after laparoscopic sleeve gastrectomy versus laparoscopic Roux-en-Y gastric bypass: a randomized controlled trial focusing on gastroesophageal reflux disease. Obes Surg . doi: 10.1007/s11695-017-2688-4.
Monteiro F, Ponce DA, Silva H, et al. Physical function, quality of life, and energy expenditure during activities of daily living in obese, post-bariatric surgery, and healthy subjects. Obes Surg. 2017;27(8):2138–44.
Osterhues A, von Lengerke T, Mall JW, de Zwaan M, Müller A, 2017. Health-related quality of life, anxiety, and depression in bariatric surgery candidates compared to patients from a psychosomatic inpatient hospital. Obes Surg. doi: 10.1007/s11695-017-2629-2.
Ware JE, Snow K, Kosinski M, et al. SF-36 Health Survey: manual and interpretation guide. Boston: The Health Institute, New England Medical Center; 1993.
Kolotkin RL, Crosby RD. Manual for the impact of weight on quality of life measure (IWQOL and IWQOL-Lite). Obesity and Quality of Life Consulting: Durham, NC; 2008.
De Luca M, Angrisani L, Himpens J, et al. Indications for surgery for obesity and weight-related diseases: position statements from the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO). Obes Surg. 2016;26(8):1659–96.
Runkel N, Colombo-Benkmann M, Hüttl TP, et al. Evidence-based German guidelines for surgery for obesity. Int J Color Dis. 2011;26(4):397–404.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26(2):395–409.
de Zwaan M, Hilbert A, Swan-Kremeier L, et al. Comprehensive interview assessment of eating behavior 18-35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6(1):79–85.
Gilmartin J, Bath-Hextall F, Maclean J, et al. Quality of life among adults following bariatric and body contouring surgery: a systematic review. JBI Database System Rev Implement Rep. 2016;14(11):240–70.
Coulman KD, Howes N, Hopkins J, et al. A comparison of health professionals’ and patients’ views of the importance of outcomes of bariatric surgery. Obes Surg. 2016;26(11):2738–46.
Angrisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Stroh C, Weiner R, Benedix F, et al. Adipositas- und metabolische Chirurgie in Deutschland 2012 - Ergebnisse der Qualitatssicherungsstudie zur operativen Therapie der Adipositas (GBSR). [bariatric and metabolic surgery in Germany 2012 - results of the quality assurance study on surgery for obesity (data of the German Bariatric Surgery Registry)]. Zentralbl Chir. 2014;139(2):e1–5.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg. 1998;8(5):487–99.
Oria HE, Moorehead MK. Updated bariatric analysis and reporting outcome system (BAROS). Surg Obes Relat Dis. 2009;5(1):60–6.
Weiner S, Sauerland S, Fein M, et al. The Bariatric Quality of Life index: a measure of well-being in obesity surgery patients. Obes Surg. 2005;15(4):538–45.
Tayyem RM, Atkinson JM, Martin CR. Development and validation of a new bariatric-specific health-related quality of life instrument “bariatric and obesity-specific survey (BOSS)”. J Postgrad Med. 2014;60(4):357–61.
Klassen AF, Cano SJ, Alderman A, et al. The BODY-Q: a patient-reported outcome instrument for weight loss and body contouring treatments. Plast Reconstr Surg Glob Open. 2016;4(4):e679.
Klassen AF, Cano SJ, Scott A, et al. Satisfaction and quality-of-life issues in body contouring surgery patients: a qualitative study. Obes Surg. 2012;22(10):1527–34.
Klassen AF, Cano SJ, Scott A, et al. Assessing outcomes in body contouring. Clin Plast Surg. 2014;41(4):645–54.
Ivezaj V, Kessler EE, Lydecker JA, et al. Loss-of-control eating following sleeve gastrectomy surgery. Surg Obes Relat Dis. 2017;13(3):392–8.
Devlin MJ, King WC, Kalarchian MA, et al. Eating pathology and experience and weight loss in a prospective study of bariatric surgery patients: 3-year follow-up. Int J Eat Disord. 2016;49(12):1058–67.
Mitchell JE, Christian NJ, Flum DR, et al. Postoperative behavioral variables and weight change 3 years after bariatric surgery. JAMA Surg. 2016;151(8):752–7.
Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11(3):193–205.
Selle J. Entwicklung eines gesundheitsbezogenen Lebensqualitätsfragebogens bei Adipositaschirurgie [development of a HRQOL questionnaire for bariatric surgery]. Doctoral thesis. Hannover Medical School: Hannover; 2017.
Herpertz S, Müller A, Burgmer R, et al. Health-related quality of life and psychological functioning 9 years after restrictive surgical treatment for obesity. Surg Obes Relat Dis. 2015;11(6):1361–70.
Green DD, Engel SG, Mitchell JE. Psychological aspects of bariatric surgery. Curr Opin Psychiatry. 2014;27(6):448–52.
Müller A, Mitchell JE, Sondag C, et al. Psychiatric aspects of bariatric surgery. Curr Psychiatry Rep. 2013;15(10):397.
Driscoll S, Gregory DM, Fardy JM, et al. Long-term health-related quality of life in bariatric surgery patients: a systematic review and meta-analysis. Obesity (Silver Spring). 2016;24(1):60–70.
Aasprang A, Andersen JR, Vage V, et al. Five-year changes in health-related quality of life after biliopancreatic diversion with duodenal switch. Obes Surg. 2013;23(10):1662–8.
Mayring P. Qualitative Inhaltsanalyse. Beltz: Weinheim und Basel; 2010.
Morfeld M, Kirchberger I, Bullinger M. SF-36 Fragebogen zum Gesundheitszustand: Deutsche Version des Short Form-36 Health Survey. Göttingen: Hogrefe; 2011.
Kolotkin RL, Crosby RD, Williams GR. Assessing weight-related quality of life in obese persons with type 2 diabetes. Diabetes Res Clin Pract. 2003;61(2):125–32.
Kolotkin RL, Crosby RD, Kosloski KD, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11.
Mueller A, Holzapfel C, Hauner H, et al. Psychometric evaluation of the German version of the impact of weight on Quality of Life-Lite (IWQOL-Lite) questionnaire. Exp Clin Endocrinol Diabetes. 2011;119(2):69–74.
Hilbert A, Tuschen-Caffier B. Eating disorder examination—questionnaire. Deutsche Übersetzung. Verlag für Psychotherapie: Münster; 2006.
Herrmann-Lingen C, Buss U, Snaith RP. Hospital anxiety and depression scale: Deutsche version. Bern: Huber; 2011.
Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30:179–85.
Hattie J, Cooksey RW. Procedures for assessing the validities of tests using the “known-groups” method. Appl Psychol Meas. 1984;8(3):295–305.
Giel KE, Thiel A, Teufel M, et al. Weight bias in work settings—a qualitative review. Obes Facts. 2010;3(1):33–40.
Giel KE, Zipfel S, Alizadeh M, et al. Stigmatization of obese individuals by human resource professionals: an experimental study. BMC Public Health. 2012;12:525.
Sarwer DB, Fabricatore AN, Eisenberg MH, et al. Self-reported stigmatization among candidates for bariatric surgery. Obesity (Silver Spring). 2008;16(Suppl 2):S75–9.
Vartanian LR, Fardouly J. The stigma of obesity surgery: negative evaluations based on weight loss history. Obes Surg. 2013;23(10):1545–50.
Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. J Abnorm Psychol. 2005;114(1):119–25.
van den Berg PA, Mond J, Eisenberg M, et al. The link between body dissatisfaction and self-esteem in adolescents: similarities across gender, age, weight status, race/ethnicity, and socioeconomic status. J Adolesc Health. 2010;47(3):290–6.
de Zwaan M, Georgiadou E, Stroh CE, et al. Body image and quality of life in patients with and without body contouring surgery following bariatric surgery: a comparison of pre- and post-surgery groups. Front Psychol. 2014;5:1310.
Fabricatore AN, Wadden TA, Sarwer DB, et al. Health-related quality of life and symptoms of depression in extremely obese persons seeking bariatric surgery. Obes Surg. 2005;15(3):304–9.
APA. Diagnostic and Statistical Manual of mental disorders. 5th ed. Washington DC: American Psychiatric Press; 2013.
Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clin Child Fam Psychol Rev. 2012;15(1):4–13.
Tack J, Arts J, Caenepeel P, et al. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol. 2009;6(10):583–90.
van Beek AP, Emous M, Laville M, et al. Dumping syndrome after esophageal, gastric or bariatric surgery: pathophysiology, diagnosis, and management. Obes Rev. 2017;18(1):68–85.
Kalarchian MA, Marcus MD, Courcoulas AP, et al. Self-report of gastrointestinal side effects after bariatric surgery. Surg Obes Relat Dis. 2014;10(6):1202–7.
Ramadan M, Loureiro M, Laughlan K, et al. Risk of dumping syndrome after sleeve gastrectomy and Roux-en-Y gastric bypass: early results of a multicentre prospective study. Gastroenterol Res Pract. 2016;2016:2570237.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Ethical Approval
All procedures were in accordance with the ethical standards of the institutional research committee of the Hannover Medical School and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This work was supported by a grant from the Federal Ministry of Education and Research within the German Obesity Competence Network (01GI1324) and by the Else-Kröner-Fresenius Foundation as part of the structured doctoral program “ClinStrucMed.”
Rights and permissions
About this article
Cite this article
Müller, A., Crosby, R.D., Selle, J. et al. Development and Evaluation of the Quality of Life for Obesity Surgery (QOLOS) Questionnaire. OBES SURG 28, 451–463 (2018). https://doi.org/10.1007/s11695-017-2864-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2864-6