Abstract
Background
Non-anesthesia administered propofol (NAAP) has been shown to be a safe and effective method of sedation for patients undergoing gastrointestinal endoscopy. Bariatric surgery patients are potentially at a higher risk for sedation-related complications due to co-morbidities including obstructive sleep apnea. The outcomes of NAAP in bariatric patients have not been previously reported.
Methods
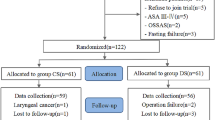
In this retrospective cohort study, severely obese patients undergoing pre-surgical outpatient esophagogastroduodenoscopy (EGD) were compared to non-obese control patients (BMI ≤ 25 kg/m2) undergoing diagnostic EGD at our institution from March 2011–September 2015 using our endoscopy database. Patients’ demographics and procedural and recovery data, including any airway interventions, were statistically analyzed.
Results
We included 130 consecutive pre-operative bariatric surgical patients with average BMI 45.8 kg/m2 (range 34–80) and 265 control patients with average BMI 21.9 kg/m2 (range 14–25). The severely obese group had a higher prevalence of sleep apnea (62 vs 8%; p < 0.001), experienced more oxygen desaturations (22 vs 7%; p < 0.001), and received more chin lift maneuvers (20 vs 6%; p < 0.001). Advanced airway interventions were rarely required in either group and were not more frequent in the bariatric group.
Conclusions
With appropriate training of endoscopy personnel, NAAP is a safe method of sedation in severely obese patients undergoing outpatient upper endoscopy.
Similar content being viewed by others
References
Berzin TM, Sanaka S, Barnett SR, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73(4):710–7. doi:10.1016/j.gie.2010.12.011.
Coté GA, Hovis RM, Ansstas MA, et al. Incidence of sedation-related complications with propofol use during advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010;8(2):137–42. doi:10.1016/j.cgh.2009.07.008.
Wani S, Azar R, Hovis CE, et al. Obesity as a risk factor for sedation-related complications during propofol-mediated sedation for advanced endoscopic procedures. Gastrointest Endosc. 2011;74(6):1238–47. doi:10.1016/j.gie.2011.09.006.
White PF. Intravenous (non-opioid) anesthesia. Seminars in Anesthesia, Perioperative Medicine and Pain. 2005;24(2):101–7.
Lera dos Santos ME, Maluf-Filho F, Chaves DM, et al. Deep sedation during gastrointestinal endoscopy: propofol-fentanyl and midazolam-fentanyl regimens. World J Gastroenterol. 2013;19(22):3439–46. doi:10.3748/wjg.v19.i22.3439.
Ferreira AO, Cravo M. Sedation in gastrointestinal endoscopy: where are we at in 2014? World J Gastrointest Endosc. 2015;7(2):102–9. doi:10.4253/wjge.v7.i2.102. Review
Wang D, Chen C, Chen J, et al. The use of propofol as a sedative agent in gastrointestinal endoscopy: a meta-analysis. PLoS One. 2013;8(1):e53311. doi:10.1371/journal.pone.0053311.
Sieg A, bng-Study-Group, Beck S, et al. Safety analysis of endoscopist-directed propofol sedation: a prospective, national multicenter study of 24 441 patients in German outpatient practices. J Gastroenterol Hepatol. 2014;29(3):517–23.
Tohda G, Higashi S, Wakahara S, et al. Propofol sedation during endoscopic procedures: safe and effective administration by registered nurses supervised by endoscopists. Endoscopy. 2006;38:360–7.
Rex DK, Overley C, Kinser K, et al. Safety of propofol administered by registered nurses with gastroenterologist supervision in 2000 endoscopic cases. Am J Gastroenterol. 2002;97(5):1159–63.
Külling D, Rothenbühler R, Inauen W. Safety of nonanesthetist sedation with propofol for outpatient colonoscopy and esophagogastroduodenoscopy. Endoscopy. 2003;35(8):679–82.
Sieg A. Propofol sedation in outpatient colonoscopy by trained practice nurses supervised by the gastroenterologist: a prospective evaluation of over 3000 cases. Z Gastroenterol. 2007;45(8):697–701.
American Society for Gastrointestinal Endoscopy, the American Association for the Study of Liver Diseases, American College of Gastroenterology, and AGA Institute. Position statement: nonanesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc. 2009;70(6).
National Center for Health Statistics. Health, United States, 2014: with special feature on adults aged 55–64. Hyattsville; 2015.
Kim WH, Ahn HJ, Lee CJ, et al. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth. 2011;106(5):743–8. doi:10.1093/bja/aer024.
Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812–21. doi:10.1097/ALN.0b013e31816d83e4.
Chung F, Yang Y, Liao P. Predictive performance of the STOP-Bang score for identifying obstructive sleep apnea in obese patients. Obes Surg. 2013;23(12):2050–7. doi:10.1007/s11695-013-1006-z.
Chung F, Yegneswaran B, Liao P, et al. Validation of the Berlin questionnaire and American Society of Anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108(5):822–30. doi:10.1097/ALN.0b013e31816d91b5.
Courcoulas AP, Yanovski SZ, Bonds D, et al. Long-term outcomes of bariatric surgery: a National Institutes of Health symposium. JAMA Surg. 2014;149(12):1323–9. doi:10.1001/jamasurg.2014.2440. Review
Adler DG, Kawa C, Hilden K, et al. Nurse-administered propofol sedation is safe for patients with obstructive sleep apnea undergoing routine endoscopy: a pilot study. Dig Dis Sci. 2011;56(9):2666–71. doi:10.1007/s10620-011-1645-7.
Khiani VS, Salah W, Maimone S, et al. Sedation during endoscopy for patients at risk of obstructive sleep apnea. Gastrointest Endosc. 2009;70(6):1116–20. doi:10.1016/j.gie.2009.05.036.
Mehta PP, Kochhar G, Kalra S, et al. Can a validated sleep apnea scoring system predict cardiopulmonary events using propofol sedation for routine EGD or colonoscopy? A prospective cohort study. Gastrointest Endosc. 2014;79(3):436–44. doi:10.1016/j.gie.2013.09.022.
Heuss LT, Schnieper P, Drewe J, et al. Safety of propofol for conscious sedation during endoscopic procedures in high-risk patients—a prospective, controlled study. Am J Gastroenterol. 2003;98(8):1751–7.
Kawa C, Stewart J, Hilden K, et al. A retrospective study of nurse-assisted propofol sedation in patients with amyotrophic lateral sclerosis undergoing percutaneous endoscopic gastrostomy. Nutr Clin Pract. 2012;27(4):540–4. doi:10.1177/0884533612443712.
American Society of Anesthesiologists. Statement on safe use of propofol. Committee of Origin: ambulatory surgical care. 2004. www.asahq.org.
American Association of Nurse Anesthetists. AANA-ASA joint position statement regarding propofol administration. Adopted April 14, 2004. www.aana.com.
Author Contributions
All listed authors have put forth substantial contributions to this manuscript including revisions, final approval, and agreement to be accountable for all aspects of the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Fang is a consultant to Boston Scientific, Covidien, and Obalon Therapeutics. He is also the owner of Veritract. Dr. McVay, Linda Taylor, Alex Au, Wesley Williams, Angela Presson, Ragheed Al-Dulaimi, Dr. Volckmann, and Dr. Ibele declare that they have no conflict of interest.
Informed Consent
Due to the retrospective design of this study, informed consent was not obtained but was assumed. Patients were not notified.
Human and Animal Rights
Our institutional review board at the University of Utah determined that our study qualified as exempt research, specifically meeting the criteria for non-Federal exemption category 7, which includes research involving the collection or study of existing data, documents, records, pathological specimens, or diagnostic specimens, where this information is personally identifiable or coded.
Funding
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764).
Rights and permissions
About this article
Cite this article
McVay, T., Fang, J.C., Taylor, L. et al. Safety Analysis of Bariatric Patients Undergoing Outpatient Upper Endoscopy with Non-Anesthesia Administered Propofol Sedation. OBES SURG 27, 1501–1507 (2017). https://doi.org/10.1007/s11695-016-2478-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2478-4