Abstract
Background
Roux-en-Y gastric bypass (RYGB) may improve beta cell function by mechanisms other than caloric restriction and body weight loss. We aimed to assess the impact of anatomical and hormonal alterations specific to RYGB on glucose homeostasis, β cell function and morphology.
Methods
Male Zuckerfa/fa rats underwent either RYGB (n = 11) or sham surgeries (n = 10). Five of the shams were then food restricted and body weight matched (BWM) to the RYGB rats. Six male Zuckerfa/+ rats underwent sham surgery and served as additional lean controls. Twenty-seven days after surgery, an oral glucose tolerance test (OGTT) was performed and plasma levels of glucose, insulin and glucagon-like peptide-1 (GLP-1) were measured. Immunohistological analysis of pancreatic islets was performed, and GLP-1 receptor and PDX-1 mRNA content were quantified.
Results
Shams consumed more food and gained more weight compared to both RYGB and BWM (p < 0.001). Hyperglycaemia was evident in ad libitum-fed shams, whilst postprandial glucose levels were lower in RYGB compared to the BWM sham group (p < 0.05). During the OGTT, RYGB rats responded with >2.5-fold increase of GLP-1. Histology revealed signs of islet degeneration in ad libitum-fed shams, but not in RYGB and sham BWM controls (p < 0.001). GLP-1 receptor and PDX-1 mRNA content was similar between the RYGB and BWM shams but higher compared to ad libitum shams (p < 0.05).
Conclusions
Combined molecular, cellular and histological analyses of pancreatic function suggest that weight loss alone, and not the enhancement of GLP-1 responses, is predominant for the short-term β cell protective effects of RYGB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a debilitating condition that has reached pandemic proportions, and its incidence shows no sign of diminishing [1]. Bariatric surgery is the most successful treatment currently available used to combat T2DM in obese patients [2–4] and has been shown to prevent the development of T2DM in patients diagnosed with impaired glucose tolerance [5], to arrest disease progression [6, 7] and even to induce diabetes remission in approximately 40 % of patients in the long term [7, 8].
The immediate time course in restoration of glycemic control after Roux-en-Y gastric bypass (RYGB), the most commonly performed bariatric procedure worldwide, has led to conclusion that additional processes are involved beyond caloric restriction and body weight loss [9]. Proposed mechanisms include a postoperatively enhanced incretin response, of which glucagon-like peptide-1 (GLP-1) is best characterized [10, 11], alterations in bile flow [12, 13], nutrient sensing [14–16] and the gut microbiome [17, 18]. Indeed, there is substantial evidence that the exaggerated GLP-1 response is important for improved β cell function and glucose tolerance in patients with T2DM after RYGB [10]. Furthermore, GLP-1 receptor agonist responsiveness is predictive of the efficacy of RYGB on glucose tolerance in rats [19]. It has also been reported that GLP-1 could prevent β cell apoptosis [10, 11] and increase β cell mass resulting in improved glucose control in the long term.
In opposition to the incretin hypothesis, there is also evidence supporting that caloric restriction and weight loss per se are the predominant factors underlying the favourable effects on glucose control observed after RYGB. Indeed, a very low calorie diet in human volunteers can mimic the early beneficial effects of RYGB on insulin sensitivity and β cell function [20]. It has further been shown that patients who achieve similar weight loss after gastric banding, a procedure which does not affect the incretin response, and RYGB exhibit similarly improved insulin sensitivity and β cell function [21]. GLP-1 receptor antagonism has also been reported to not fully reverse the favourable effects on glycaemic control after RYGB in T2DM patients [22]. In fact, in the long term, weight loss maintenance has been identified as a critical factor for T2DM control after RYGB [23, 24].
In view of these controversies in the literature, it is important to clarify the relative contribution of RYGB-induced reduction in food intake and weight loss versus its hormonal effects on pancreatic morphology and function. RYGB surgery in rodents is an established model to help to elucidate these mechanisms [25, 26], and the Zuckerfa/fa rat presents an ideal mutant model as it develops progressive obesity, insulin resistance, hyperglycaemia and hyperinsulinaemia [27, 28].
In this study, we compared male Zuckerfa/fa rats that underwent RYGB to sham-operated rats that were either body weight matched (BWM) to the RYGB group or received food ad libitum, and to lean controls (Zuckerfa/+). Assessments included (a) postprandial glycaemic control and GLP-1 release, (b) pancreatic islet morphometry and (c) gene expression analysis of GLP-1 receptor and pancreatic and duodenal homeobox 1 (PDX1), which is essential for integrating GLP-1 receptor-dependent signals regulating the growth, differentiated function and survival of pancreatic β cells.
Methods
Animals and Experimental Design
Twenty-one male Zuckerfa/fa rats and six male Zuckerfa/+ rats with mean body weights of 327 ± 18 and 279 ± 11 g, respectively, were purchased from Charles River, France, at 6 weeks of age. Animals were individually housed under ambient humidity and temperature for 22 °C in a 12-h light/dark cycle. Animals had free access to tap water and Purina 5008 Lab diet (Purina Mills, USA, 16.7 % of calories from fat) unless stated otherwise. At 12 weeks of age, ZDFfa/fa rats (463.6 ± 14.6 g) were randomly divided into three groups and allocated to RYGB or sham surgeries. After surgeries, RYGB (n = 11) and sham-operated rats (n = 5) were fed ad libitum. Five sham-operated rats were calorie restricted and received the amount of calories necessary to achieve the same body weight as the RYGB group. Six Zuckerfa/+ rats (348.7 ± 26.3 g) also underwent sham surgery and were used as lean controls.
Food intake (FI) and body weight were measured daily. As regulation of glucose control and the secretion of the gastrointestinal peptide hormones are under circadian rhythm [29], we measured food intake every 2 h in lean control, sham ad libitum and RYGB rats on postoperative days 10 and 15 (Fig. 1b, c). Based on these results, we administered 33 % of the daily food intake to the sham BWM during the light phase and 66 % at the beginning of the dark phase. We performed all metabolic measurements at the beginning of the dark phase in order to avoid possible confounders related to diurnal variation.
a Body weight; b, c detailed daily food intake (%); d average daily food intake; e faecal analysis and f visceral fat content in all groups. Lean control Zuckerfa/+ (peach triangle, n = 6), sham ad libitum-fed Zuckerfa/fa (square, n = 5), RYGB Zuckerfa/fa (black triangle, n = 11) and sham BWM Zuckerfa/fa (diamond, n = 5). Data are shown as mean ± SEM
Faeces were collected over 24 h on postoperative days 14 and 21 from all animals, dried in an oven and weighed. Faecal dry weight in relation to daily FI was calculated. Faecal energy content (kcal/g) was measured using ballistic bomb calorimetry. All animal experiments were in compliance with the guidelines on animal welfare of the European Union and reviewed and approved by the Animal Care Committee of the local government of Unterfranken, Bavaria, Germany (Licence 55.2-2531.01-72/12).
Surgery and Perioperative Care
Rats were food deprived for 6 h pre-operatively. Surgical anaesthesia was induced and maintained with isoflurane/O2 mixture. Animals were placed on a heating pad during surgery. Prior to surgery, animals were given 5 mg/kg carprofen subcutaneously. The abdomen was opened using a midline laparotomy and closed using continuous suturing.
Sham Surgery
The small bowel and gastro-oesophageal junction were mobilized, and a gastrostomy on the anterior wall of the stomach and a jejunostomy with subsequent closure were performed. Eleven rats underwent sham surgery and were included in the study.
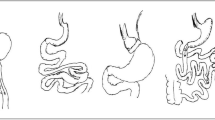
RYGB Surgery
Surgery was performed according to a standardized protocol which has been shown to result in reduced food intake and long-term stabilized weight loss [30]. Briefly, the jejunum was transected 16 cm aboral to the pylorus to create the biliopancreatic limb. The stomach was divided 3 mm below the gastro-oesophageal junction to create a small pouch. The stomach remnant was subsequently closed. The aboral jejunum was anastomosed end-to-side to the small pouch. At the level of the lower jejunum, a 7-mm side-to-side jejuno-jejunostomy between the biliopancreatic limb and the alimentary limb was performed creating a common channel of ∼25 cm in length.
Metabolic Measurements
An oral glucose tolerance test (OGTT) was performed at the beginning of the dark cycle on postoperative day 27 in all animals. In order to avoid oral gavage and therefore to reduce discomfort and pressure on the upper anastomosis, animals were trained to drink 10 ml/kg body weight of a 25 % glucose solution within 10 min after an overnight fast on two occasions before the OGTT was performed. After an 8-h overnight fast, blood glucose was measured (Breeze 2® glucometer, Bayer, Zurich, Switzerland) in conscious rats at baseline and 15, 30, 60 and 120 min after glucose ingestion. Blood was obtained from the tail vein by a small incision. A drop of blood was applied directly to a glucometer, and 100 μl was collected at each time point in tubes containing EDTA and a dipeptidyl peptidase-4 inhibitor. The plasma fraction was separated by centrifugation at 4 °C for 8000 rpm and stored at −80 °C. Total insulin and GLP-1 were measured using the Ultrasensitive Rat Insulin ELISA (Merodia AB, Sweden 10-1251-10) and the GLP-1 ELISA kit (#EZGLP1T-36 K) from EMD Millipore (www.merck.millipore.com), respectively.
Tissue Harvesting
Animals were sacrificed 45 min after a fixed meal of 3 g Purina 5008 diet. For tissue harvesting, a midline laparotomy was performed and the pancreas was removed within 2 min in order to avoid tissue degeneration. It has previously been shown that retroperitoneal and epididymal fat strongly correlate with visceral adiposity. Therefore, the retroperitoneal and epididymal white adipose tissue pads were then dissected according to a standardized protocol in order to determine visceral adiposity [31]. The aorta was considered as the medial, the fascia transversalis the lateral and the psoas muscle the dorsal dissection border. The retroperitoneal and epididymal white adipose tissue pads were dissected and weighed.
Immunohistochemistry
Fresh pancreatic tissues were fixed with 4 % paraformaldehyde for 24–30 h at room temperature and embedded in paraffin. Paraffin blocks were cut into 2-μm-thick sections and mounted up on aminopropylethoxysilane (APES)-coated slides. Slides were rehydrated in descending concentrations of ethanol before being heated for antigen unmasking in 10 mmol/l sodium citrate buffer (pH 6.0) in a microwave oven at 600 W for 5 min. After rinsing in distilled water, inhibition of endoperoxidase was performed by incubating sections for 10 min in 3 % H2O2 in methanol. Slides were washed in phosphate-buffered saline (PBS) and incubated with 1 % goat serum and 3 % bovine serum albumin/phosphate-buffered saline (BSA/PBS) for 10 min. Subsequently, slides were incubated with anti-insulin antibody (clone IN-05, stock solution 1 mg/ml; Exbio, Vestec, Czech Republic) diluted in antibody diluent (DAKO, Hamburg, Germany) at 4 °C overnight. Slides were washed in PBS and incubated with the horseradish-labelled rabbit anti-mouse IgG (DAKO, diluted 1:100 in 30 % rat serum). Staining was developed by adding 3,3′ diaminobenzidine (DAB ready to use, DAKO) and counterstained using haematoxylin. Afterwards, sections were washed with Aqua dest and then embedded in Aquatex (Merck Millipore, Germany).
In order to quantify these results, the pancreata were sliced and two slices each of three representative regions of the pancreata were analysed. Special care was taken to ensure that pancreatic slices chosen for quantifications derived from comparable regions of the organ. The slices were digitalized, and a Keyence BZ9000 Generation II-based hybrid cell counting technology was used for further analysis. The islets were marked manually under a 20-fold magnification and measured using hue extraction (Fig. 3a). The pancreas area of each slice was marked and quantified using brightness extraction, and the islet size relative to the pancreas surface was then calculated. The next step was to manually mark the beta cells of each islet separately in order to calculate the β cell/islet ratio (Fig. 3b). Stereological assessment of the islets’ size and β cell density was performed by two independent researchers who were blinded to the group allocation of the rats.
Real-Time Quantitative Polymerase Chain Reaction (RT-qPCR)
Fresh pancreatic tissues were homogenized in Trizol reagent purchased from Invitrogen Life Technologies (Darmstadt, Germany) using the TissueLyser system of Qiagen (Hilden, Germany). Total RNA was extracted from Trizol as recommended by Invitrogen. RNA integrity was verified using the Experion automated electrophoresis station from Bio-Rad Laboratories Inc. (München, Germany), and the RNA concentration was measured at 260 nm. For first-strand cDNA synthesis, 1 μg total RNA was employed using the iScript cDNA synthesis kit from Bio-Rad. The cDNA synthesis of 1:5 diluted cDNA was performed by heating at 25 °C for 5 min, at 42 °C for 30 min and at 85 °C for 5 min. Quantitative PCR (qPCR) was performed with MESA Green qPCR MasterMix Kit for SYBR Green containing MeteorTaq hotstart DNA polymerase (Eurogentic GmbH, Köln, Germany). The following primer pairs were used: GLP-1 receptor (GLP-1R, access No: NM_012728.1), forward: ACC ACT GCA CAG ACC CAA GTC, reverse: TCT CCA GCT CTT GGA GTC TTT CTT (90 bp); Pdx-1 (access No: NM_022852.3), forward: AAA CGC CAC ACA CAA GGA GAA, reverse: AGA CCT GGC GGT TCA CAT G (151 bp); beta-2-microglobulin (B2M; access No. NM_012512.2), forward: CCG TGA TCT TTC TGG TGC TT, reverse: ATT TGA GGT GGG TGG AAC TG (148 bp); β-actin (access No. NM_031144.2), forward: CGG CAA TGA GCG GTT CC, reverse: TGC CAC AGG ATT CCA TAC CC (71 bp).
The qPCR reactions were performed on a CFX96 real-time PCR system (Bio-Rad) operated by CFX Manager Software (version 3.0). The cycler protocol was 5 min at 95 °C, 40 cycles with 15 s at 95 °C, 60 s at 60 °C and 5 min at 72 °C. GLP-1R and Pdx-1 expression was normalized to the reference genes B2M and β-actin, and fold expression was calculated with the ∆∆Cq method.
Statistics
Statistical analysis was performed using SPSS 17.0 and GraphPad PRISM Version 7®. Normality of study variables was assessed by the Kolmogorov-Smirnov normality test. Continuous variables with normal distribution are expressed as mean ± standard error of the mean (SEM) and with non-normal distribution as median and interquartile range. Body weight changes were analysed using generalized estimating equations. For the OGTTs, area under the curve (AUC) for glucose, insulin and GLP-1 was calculated using the trapezoidal method and compared between the groups using a one-way analysis of variance (ANOVA) followed by a Bonferroni post hoc test. A two-way ANOVA was used to compare differences between the groups at specific time points during the OGTT. Statistical significance was determined at p < 0.05.
Results
Body Weight
Body weight results are summarized in Fig. 1a and Table 1. Pre-intervention body weights were 463.6 ± 14.6 g for the Zuckerfa/fa and 348.7 ± 26.3 g for the Zuckerfa/+ rats, respectively. RYGB and sham-operated ZDFfa/fa rats started to lose weight immediately after surgery. Sham-operated ad libitum-fed rats made a rapid recovery by postoperative day 3, and RYGB and sham BWM rats weighed significantly less than sham ad libitum-fed animals from postoperative day 7 until the end of the study at day 27. Lean controls had a significantly lower baseline body weight compared to all other rats but consequently gained weight ending up with a similar body weight to RYGB and sham BWM rats.
Food Intake
Average daily food intake during the 27 postoperative days is summarized in Fig. 1d and Table 1. Food intake among the groups was consistently lower after RYGB and sham BWM in comparison to all other groups (Fig. 1d, Table 1). Lean controls consumed significantly more food than RYGB and sham BWM but significantly less food compared to sham ad libitum-fed animals (Fig. 1d, Table 1).
Faecal Energy Content
No difference was observed in dry 24-h faecal mass between RYGB and either of the control groups (Fig. 1e, Table 1).
Visceral Adiposity
Visceral adiposity in sham ad libitum-fed rats was significantly higher compared to all other groups (Fig. 1f, Table 1). Visceral adiposity was similar between RYGB and sham BWM but still significantly higher than lean controls (Fig. 1f, Table 1).
Metabolic Measurements
OGTT
Glucose AUC was significantly lower in RYGB compared to both sham groups but significantly higher compared to the lean controls. Insulin AUC was significantly lower in RYGB compared to sham ad libitum group but similar between RYGB and sham BWM rats. Insulin AUC was significantly lower in lean controls compared to all other groups. GLP-1 AUC was higher in RYGB compared to all other groups. Results are summarized in Table 1 and Fig. 2a–c.
Oral glucose tolerance test in all groups on POD 27. a Glucose serum levels, b insulin serum levels and c GLP-1 serum levels. Lean control Zuckerfa/+ (peach triangle, n = 6), sham ad libitum-fed Zuckerfa/fa (square, n = 5), RYGB Zuckerfa/fa (black triangle, n = 11) and sham BWM Zuckerfa/fa (diamond, n = 5). Data are shown as mean ± SEM. Asteriks represent pairwise comparsions (RYGB vs. all other control groups) measured by two way ANOVA. * p < 0.05; ** p < 0.01; ***p < 0.001
Pancreatic Islet Morphometry
The β cell/islet ratio was similar between the RYGB, sham BWM and lean controls. The β cell/islet ratio of sham ad libitum was significantly lower compared to all other groups (Table 1, Fig. 3a–c).
Scheme of pancreas immunohistological finding analysis. a Pancreata were sliced and two slices each of three representative regions of the pancreata were analysed. b The slices were digitalized, and a Keyence BZ9000 Generation II-based hybrid cell counting technology was used for further analysis. The islets were marked manually under a 20-fold magnification and measured using hue extraction. The pancreas area of each slice was marked and quantified using brightness extraction, and the c β cell/ islet ratio was calculated. d GLP-1 receptor and e PDX-1 gene expression of the pancreas measured by RT-qPCR. Lean control Zuckerfa/+ (peach, n = 6), sham ad libitum-fed Zuckerfa/fa (white, n = 5), RYGB Zuckerfa/fa (dark gray, n = 11) and sham BWM Zuckerfa/fa (light gray, n = 5). Data are shown as mean ± SEM
Gene Expression
GLP-1 receptor mRNA content in the pancreatic β cells was significantly higher in RYGB compared to lean controls, but no significant differences were found among RYGB, sham ad libitum and sham BWM animals (Fig. 3d–e, Table 1). PDX-1 gene expression was significantly higher after RYGB compared to sham ad libitum-fed rats, but no significant differences were found among the other groups.
Discussion
In the present study, we have shown that in our RYGB model performed on obese and hyperglycaemic ZDFfa/fa rats, there is a distinct plasma glucose profile in response to an oral glucose load with an immediate increase in blood glucose levels (within 15 min) followed by a rapid decrease (within 30 min). These results entirely mirror what was seen previously in a model of RYGB and vertical sleeve gastrectomy (VSG) performed on diet-induced obese rats following an oral mixed meal load [32] and can be explained by the earlier postprandial absorption of glucose quickly followed by the enhancement of incretin-induced insulin secretion. Additionally, the approximately threefold increase of circulating GLP-1 compared to the baseline we have observed is very similar to observations made in humans [25]. In contrast, after the oral glucose load, sham-operated lean controls remained euglycaemic, whilst sham ad libitum-fed rats exhibited impaired glucose tolerance and prolonged hyperinsulinaemia, which are consistent with previous observations [32].
The novelty of our approach lies in the assessment of pancreatic islets including β cell/islet ratio and islet GLP-1 receptor and PDX-1 expression after RYGB in comparison to food restriction-induced weight loss. Pancreatic morphology showed evidence of islet degeneration in the sham ad libitum animals. Reduced food intake and body weight loss, as achieved in both the RYGB and shams BWM groups, were sufficient to prevent islet degeneration. The islet morphology of these animals was similar to that of metabolically healthy lean controls.
In addition, GLP-1 receptor and PDX-1 gene expression was higher after RYGB compared to sham ad libitum controls but similar between the RYGB and sham BWM groups. It has previously been shown that PDX-1 expression is essential for integrating GLP-1 receptor-dependent signals regulating the growth, differentiated function and survival of β cells [33]. The increase in PDX-1 after RYGB could be a consequence of the enhanced GLP-1 release.
It is remarkable that despite the enhanced postprandial GLP-1 responses after RYGB, there were no significant differences in any of these parameters between the RYGB and sham BWM group. Previously, in a model of RYGB and VSG performed on diet-induced obese rats, improvements in glucose homeostasis appeared to be primarily attributable to significantly improved hepatic insulin sensitivity compared to both sham-operated and pair-fed controls in an acute setting [32].
Interestingly, the improved glucose clearance after a mixed meal seen in RYGB and VSG rats is only significantly affected in the latter surgical group following systemic administration of a GLP-1R antagonist [32]. However, in a model of VSG in GLP-1R knock out mice, reductions in food intake and bodyweight as well as in plasma glucose and improved insulin profiles were shown to be the same as in wild-type controls [34]. It remains to be determined if improvements in glucose homeostasis after RYGB are maintained, as with bodyweight, in GLP-1R knock out mice [35]. Collectively, these results suggest that reduced caloric intake and weight loss are the predominant factors underlying the preservation of pancreatic islets and their function after RYGB and possibly also VSG. These observations can be addressed in future studies.
Our findings are strengthened by the inclusion of sham ad libitum and lean control groups, matched feeding regimes between the groups and performance of metabolic measurements at the beginning of the dark phase in order to avoid possible confounders related to diurnal variation [29]. In addition, at the time of metabolic measurements and tissue harvesting, the body weights of RYGB, sham lean controls and sham BWM animals were similar. The physiological (body weight, food intake, caloric absorption) and metabolic (glucose, insulin and GLP-1) responses of our RYGB model closely mimicked those of obese humans with T2DM after RYGB surgery [25].
Our results are in contrast to the increased β cell mass demonstrated in a porcine model of RYGB [36]. These conflicting results may be explained not only by differences between the species but also by fundamental differences in the experimental setup. Thus, the described porcine model was not hyperglycaemic, the RYGB group was very small, did not lose any weight and there were no ad libitum-fed and lean control groups available for comparison [37, 38].
Our study is limited by the fact that the rats we used did not have advanced T2DM, a feature which may have avoided the detection of differences between the RYGB and sham BWM groups. In addition, we cannot exclude that we may have not detected differences among the groups which may have become evident during a longer follow-up. Additional experiments on isolated β cells, such as a comprehensive screen on changes in gene expression, would provide further insight into changes after surgery compared to BWM rats. These further experiments were, however, beyond the remit of our study.
We elected not to measure homeostatic model assessment insulin resistance (HOMA-IR) as it would have led to misleading results due to technical reasons. Fasting glucose and insulin samples were not obtained before the OGTT as this would have induced stress to the animal and confounded the results of the OGTT. Instead, we obtained samples 10 min after ingestion of glucose. Due to the design of RYGB, glucose is absorbed much faster than in sham-operated rats and therefore glucose plasma concentrations, and therefore HOMA-IR, would be erroneously elevated compared to controls. Nevertheless, the combination of lower glucose AUC and insulin AUC is reassuring and suggest that insulin resistance was lower in the RYGB group compared to the sham ab libitum-fed group. This is not surprising as the RYGB group had lower body weight compared to the sham ad libitum weight group. Finally, we did not measure PYY and GIP responses to the OGTT.
In conclusion, RYGB-mediated improvements of glucose control were associated with distinct glycaemic, insulin and GLP-1 profiles, which are consistent with the human literature.
Our novel islet morphology and gene expression findings suggest that reduced caloric intake and weight loss are the predominant factors underlying the short-term β cell protective effects of RYGB surgery.
References
Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14.
Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013;309(21):2240–9.
Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366(17):1577–85.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370(21):2002–13.
Carlsson LM, Peltonen M, Ahlin S, et al. Bariatric surgery and prevention of type 2 diabetes in Swedish obese subjects. N Engl J Med. 2012;367(8):695–704.
Arterburn DE, Olsen MK, Smith VA, et al. Association between bariatric surgery and long-term survival. JAMA. 2015;313(1):62–70.
Sjostrom L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–304.
Miras AD, Risstad H, Baqai N, et al. Application of the International Diabetes Federation and American Diabetes Association criteria in the assessment of metabolic control after bariatric surgery. Diabetes Obes Metab. 2014;16(1):86–9.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–50. discussion 350–332.
Jorgensen NB, Dirksen C, Bojsen-Moller KN, et al. Exaggerated glucagon-like peptide 1 response is important for improved beta-cell function and glucose tolerance after Roux-en-Y gastric bypass in patients with type 2 diabetes. Diabetes. 2013;62(9):3044–52.
Rhee NA, Vilsboll T, Knop FK. Current evidence for a role of GLP-1 in Roux-en-Y gastric bypass-induced remission of type 2 diabetes. Diabetes Obes Metab. 2012;14(4):291–8.
Dutia R, Embrey M, O'Brien CS, Haeusler RA, Agenor KK, Homel P, McGinty J, Vincent RP, Alaghband-Zadeh J, Staels B et al.: Temporal changes in bile acid levels and 12alpha-hydroxylation after Roux-en-Y gastric bypass surgery in type 2 diabetes. Int J Obes (Lond) 2015.
Goncalves D, Barataud A, De Vadder F, Vinera J, Zitoun C, Duchampt A, Mithieux G: Bile routing modification reproduces key features of gastric bypass in rat. Annals of surgery 2015.
Breen DM, Rasmussen BA, Kokorovic A, et al. Jejunal nutrient sensing is required for duodenal-jejunal bypass surgery to rapidly lower glucose concentrations in uncontrolled diabetes. Nat Med. 2012;18(6):950–5.
Jurowich CF, Rikkala PR, Thalheimer A, et al. Duodenal-jejunal bypass improves glycemia and decreases SGLT1-mediated glucose absorption in rats with streptozotocin-induced type 2 diabetes. Ann Surg. 2013;258(1):89–97.
Saeidi N, Meoli L, Nestoridi E, et al. Reprogramming of intestinal glucose metabolism and glycemic control in rats after gastric bypass. Science. 2013;341(6144):406–10.
Erejuwa OO, Sulaiman SA, Ab Wahab MS. Modulation of gut microbiota in the management of metabolic disorders: the prospects and challenges. Int J Mol Sci. 2014;15(3):4158–88.
Li JV, Ashrafian H, Bueter M, et al. Metabolic surgery profoundly influences gut microbial-host metabolic cross-talk. Gut. 2011;60(9):1214–23.
Habegger KM, Heppner KM, Amburgy SE, et al. GLP-1R responsiveness predicts individual gastric bypass efficacy on glucose tolerance in rats. Diabetes. 2014;63(2):505–13.
Jackness C, Karmally W, Febres G, et al. Very low-calorie diet mimics the early beneficial effect of Roux-en-Y gastric bypass on insulin sensitivity and beta-cell function in type 2 diabetic patients. Diabetes. 2013;62(9):3027–32.
Bradley D, Conte C, Mittendorfer B, et al. Gastric bypass and banding equally improve insulin sensitivity and beta cell function. J Clin Invest. 2012;122(12):4667–74.
Vetter ML, Wadden TA, Teff KL, et al. GLP-1 plays a limited role in improved glycemia shortly after Roux-en-Y gastric bypass: a comparison with intensive lifestyle modification. Diabetes. 2015;64(2):434–46.
Kadera BE, Lum K, Grant J, et al. Remission of type 2 diabetes after Roux-en-Y gastric bypass is associated with greater weight loss. Surg Obes Relat Dis. 2009;5(3):305–9.
Kim S, Richards WO. Long-term follow-up of the metabolic profiles in obese patients with type 2 diabetes mellitus after Roux-en-Y gastric bypass. Ann Surg. 2010;251(6):1049–55.
Jimenez A, Ceriello A, Casamitjana R, et al. Remission of type 2 diabetes after Roux-en-Y gastric bypass or sleeve gastrectomy is associated with a distinct glycemic profile. Ann Surg. 2015;261(2):316–22.
Seyfried F, le Roux CW, Bueter M. Lessons learned from gastric bypass operations in rats. Obes Facts. 2011;4 Suppl 1:3–12.
Kasiske BL, O'Donnell MP, Keane WF. The Zucker rat model of obesity, insulin resistance, hyperlipidemia, and renal injury. Hypertension. 1992;19(1 Suppl):I110–115.
Zucker LM. Hereditary obesity in the rat associated with hyperlipemia. Ann N Y Acad Sci. 1965;131(1):447–58.
Konturek PC, Brzozowski T, Konturek SJ. Gut clock: implication of circadian rhythms in the gastrointestinal tract. J Physiol Pharmacol. 2011;62(2):139–50.
Bueter M, Abegg K, Seyfried F, et al. Roux-en-Y gastric bypass operation in rats. J Vis Exp. 2012;64, e3940.
Miras AD, Seyfried F, Phinikaridou A, et al. Rats fed diets with different energy contribution from fat do not differ in adiposity. Obes Facts. 2014;7(5):302–10.
Chambers AP, Jessen L, Ryan KK, et al. Weight-independent changes in blood glucose homeostasis after gastric bypass or vertical sleeve gastrectomy in rats. Gastroenterology. 2011;141(3):950–8.
Li Y, Cao X, Li LX, et al. beta-Cell Pdx1 expression is essential for the glucoregulatory, proliferative, and cytoprotective actions of glucagon-like peptide-1. Diabetes. 2005;54(2):482–91.
Wilson-Perez HE, Chambers AP, Ryan KK, et al. Vertical sleeve gastrectomy is effective in two genetic mouse models of glucagon-like Peptide 1 receptor deficiency. Diabetes. 2013;62(7):2380–5.
Ye J, Hao Z, Mumphrey MB, et al. GLP-1 receptor signaling is not required for reduced body weight after RYGB in rodents. Am J Physiol Regul Integ Comp Physiol. 2014;306(5):R352–362.
Lindqvist A, Spegel P, Ekelund M, et al. Gastric bypass improves beta-cell function and increases beta-cell mass in a porcine model. Diabetes. 2014;63(5):1665–71.
Camastra S, Gastaldelli A, Mari A, et al. Early and longer term effects of gastric bypass surgery on tissue-specific insulin sensitivity and beta cell function in morbidly obese patients with and without type 2 diabetes. Diabetologia. 2011;54(8):2093–102.
Kashyap SR, Daud S, Kelly KR, et al. Acute effects of gastric bypass versus gastric restrictive surgery on beta-cell function and insulinotropic hormones in severely obese patients with type 2 diabetes. Int J Obes (Lond). 2010;34(3):462–71.
Acknowledgments
The financial support by the Interdisciplinary Center for Clinical Research of Wuerzburg University (Z-3/44, FS) is gratefully acknowledged. ADM has received funding from an MRC Clinical Training Fellowship, MRC Centenary Award and an NIHR Clinical Lectureship. WF received funding from the Federal Ministry of Education and Research (BMBF), Germany, FKZ: 01EO1001
Authors’ Contributions
FS performed surgeries, researched data and wrote the manuscript. ADM researched and analysed data, edited the paper and contributed to the discussion. LR, AN and CC performed surgeries, researched data and contributed to the discussion. ADM, JVL, NS, MH and WF analysed data, reviewed/edited the paper and contributed to the discussion. CO and CJ designed the study, reviewed/edited the manuscript and were guarantors of the study. CO and CJ contributed equally to the manuscript. All authors approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with Ethical Standards
All applicable institutional and/or national guidelines for the care and use of animals were followed. All animal experiments were in compliance with the guidelines on animal welfare of the European Union and reviewed and approved by the Animal Care Committee of the local government of Unterfranken, Bavaria, Germany (Licence 55.2-2531.01-72/12).
Conflict of Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Seyfried, F., Miras, A.D., Rotzinger, L. et al. Gastric Bypass-Related Effects on Glucose Control, β Cell Function and Morphology in the Obese Zucker Rat. OBES SURG 26, 1228–1236 (2016). https://doi.org/10.1007/s11695-015-1882-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1882-5