Abstract
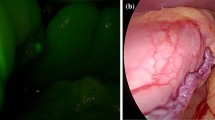
The aim of this study is to present our preliminary experience with indocyanine green fluorescence (IGF) imaging in laparoscopic sleeve gastrectomy. After dissection of the greater curve sleeve, gastrectomy is performed using a linear articulated stapler. Once the stomach is resected, an indocyanine green solution is prepared and injected in a periferic vein. A laparoscopic system with a high-definition camera system connected to a laparoscope equipped with a specific filter for optimal detection of the near-infrared fluorescence was used at all times as previously reported in a paper of Boni et al. A methylene blue test is routinely performed after near-infrared fluorescence, and a routine gastrografin upper gastrointestinal study is performed on postoperative day 2. We retrospectively identified 15 patients undergoing laparoscopic sleeve gastrectomy between April and October 2014. IGF imaging was used for all patients. A regular and homogeneous perfusion was observed along the entire gastric sleeve including the esophago-gastric junction. On the contrary, the excised specimen appeared devascularized at IGF imaging as expected. Intraoperative methylene blue test was negative in all cases. The contrast swallow did not document any leak. Neither clinical leak nor other complications occurred postoperatively (minimum follow-up of 2 months). IGF is a recent development in minimally invasive surgery. In this preliminary experience, IGF results resemble to intraoperative methylene blue test and postoperative contrast swallow ones. IGF allows a real-time assessment and gives a direct image of tissue perfusion and vascularization. Moreover, IGF may be helpful to explain the exact pathogenesis of gastric leak.
Similar content being viewed by others
References
Diamantis T, Apostolou KG, Alexandrou A, et al. Review of long-term weight loss results after laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2014;10(1):177–83.
Prevot F, Verhaeghe P, Pequignot A, et al. Two lessons from 5-year follow-up study of laparoscopic sleeve gastrectomy: persistent weight loss and a short surgical learning curve. Surgery. 2014;155(2):292–9.
Abou Rached A, Basile M, El Masri H. Gastric leaks post sleeve gastrectomy: review of its prevention and management. World J Gastroenterol. 2014;20(38):13904–10.
Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4888 patients. Surg Endosc. 2012;26(6):1509–15.
Boni L, David G, Mangano A, et al. Clinical applications of indocyanine green (ICG) enhanced fluorescence in laparoscopic surgery. Surg Endosc. 2014. doi:10.1007/s00464-014-3895-x.
Conflict of Interest
The authors declare no conflict of interest.
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
(MOV 188934 kb)
Rights and permissions
About this article
Cite this article
Frattini, F., Lavazza, M., Mangano, A. et al. Indocyanine Green-Enhanced Fluorescence in Laparoscopic Sleeve Gastrectomy. OBES SURG 25, 949–950 (2015). https://doi.org/10.1007/s11695-015-1640-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1640-8