Abstract
Background
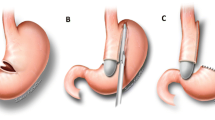
Laparoscopic sleeve gastrectomy (LSG) is an effective bariatric procedure, and it can be done as an isolated LSG or in conjunction with biliopancreatic diversion bypass/duodenal switch (laparoscopic duodenal switch; LDS). Gastroesophageal reflux after LSG has been described, but the mechanism is unknown and the treatment in the severest cases has not been discussed. We describe a cohort of patients who have underwent an LSG or LDS, and have suffered from a severe postoperative gastroesophageal motility disorder and/or reflux, report on their treatment, and discuss possible underlying mechanisms.
Methods
Seven hundred and six patients underwent an LSG by two of the authors (AK, AB). Sixty nine patients underwent laparoscopic sleeve gastrectomy in Hadassah Medical Center, Jerusalem, Israel (January, 2006 and December 2008; 55 isolated LSG, 14 with LDS), and 637 (212 isolated LSG, 425 LDS) in Clinica San Jorge and Alcoy Hospital in Alcoy, Spain, (January 2002 and November 2008).
Results
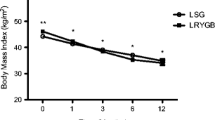
Of them, eight patients who has suffered from a gastroesophageal dysmotility and reflux disease postoperatively and needed a specific treatment besides regular proton pump inhibitors (PPIs) were identified (1.1%).
Conclusion
A combination of dilated upper part of the sleeve with a relative narrowing of the midstomach, without complete obstruction, was common to all eight patients who suffered from a severe gastroesophageal dysmotility and reflux. The sleeve volume, the bougie size, and the starting point of the antral resection do not seem to have an effect in this complication. Operative treatment was needed in only one case out of eight; in the rest of the patients, medical modalities were successful. More knowledge is required to understand the underlying mechanisms.






Similar content being viewed by others
References
Iannelli A, Dainese R, Piche T, et al. Laparoscopic sleeve gastrectomy for morbid obesity. World J Gastroenterol. 2008;14:821–7.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17:962–9.
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–96.
Frezzo EE, Freddy S, Lee LL, et al. Complications after sleeve gastrectomy for morbid obesity. Obes Surg. 2009;19(6):684–7.
Himpens J, Dapri G, Cadiere G. A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years. Obes Surg. 2006;16:1450–6.
Hamoui N, Anthone G, Kaufman H, et al. Sleeve Gastrectomy in high-risk patients. Obes Surg. 2006;16:1445–9.
Makarewicz W, Kaska L, Kobiela J, et al. Wernicke syndrome after sleeve gastrectomy. Obes Surg. 2005;17:704–6.
Parikh M, Gagner M. Laparoscopic hiatal hernia repair and repeat sleeve gastrectomy for gastroesophageal reflux disease after duodenal switch. Surg Obes Rel Dis. 2008;4:73–5.
Serra C, Baltasar A, Pérez N, et al. Total gastrectomy for the complications of the duodenal switch, with reversal. Obes Surg. 2006;16:1082–86.
Weiner RA, Weiner S, Pomhoff I, et al. Laparoscopic sleeve gastrectomy—influence of sleeve size and resected gastric volume. Obes Surg. 2007;17:1297–305.
Melissas J, Koukouraki S, Askoxylakis J, et al. Sleeve gastrectomy: a restrictive procedure? Obes Surg. 2007;17:57–62.
Bernstine H, Tzioni-Yehoshua R, et al. Gastric emptying is not affected by sleeve gastrectomy a scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg. 2009;19(3):293. doi:10.1007/s11695-008-9791-5.
Carmichael AR, Johnston D, Barker MCJ, et al. Gastric emptying after a new, more physiological anti-obesity operation: the Magenstrasse and Mill procedure. Eur J Nucl Med. 2001;28:1379–83.
Dapri G, Cadiere GB, Himpens J. Laparoscopic seromyotomy for long stenosis after sleeve gastrectomy with or without duodenal switch. Obes Surg. 2009;19(4):495–9.
Disclosure
Authors have no disclosure to make.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keidar, A., Appelbaum, L., Schweiger, C. et al. Dilated Upper Sleeve Can be Associated with Severe Postoperative Gastroesophageal Dysmotility and Reflux. OBES SURG 20, 140–147 (2010). https://doi.org/10.1007/s11695-009-0032-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-0032-3