Abstract
Objectives
Sleep duration and sleep fragmentation have been proposed to play a role in the development and progression of obesity-associated morbidity. Weight loss results in resolution of obesity-associated morbidity. Our aim was to determine the effect of weight loss on sleep architecture in adolescents with severe obesity.
Methods
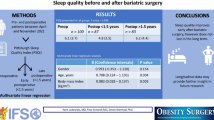
Retrospective analysis of polysomnograhic data from all adolescents who underwent overnight sleep study before and after weight loss surgery was performed. Polysomnographic variables of sleep architecture after weight loss were compared to baseline by paired Student’s t test (normally distributed data) or Wilcoxon test (variables not meeting normality criteria).
Results
The mean (±SEM) age of 19 subjects meeting inclusion criteria was 16.5 ± 0.35 years, mean body mass index was 60.3 ± 2.11 kg/m2, and 66% were female. Obstructive sleep apnea was present in 14 subjects (74%). The average interval between the baseline and repeat polysomnograms was 0.91 ± 0.16 years, and average weight loss was 66.4 ± 8.8 kg. Surgical weight loss resulted in increased sleep efficiency (80.2% vs 73.1%, p = 0.01), reduced time in stage 1 sleep (3.0% vs 6.0%, p = 0.02), and reduced arousal index (7.6 ± 0.6/h vs 11.3 ± 1.2, p = 0.01).
Conclusion
Our data demonstrate a marked improvement in sleep efficiency and sleep fragmentation with surgical weight loss. Given the emerging evidence that surgical weight loss results in resolution of obesity-associated psychosocial, metabolic, and cardiovascular morbidity, these results suggest that correction of sleep fragmentation could be an important but as yet underappreciated factor influencing changes in these other major comorbidities of obesity.

Similar content being viewed by others
References
Styne DM. Childhood and adolescent obesity. Prevalence and significance. Pediatr Clin North Am. 2001;48:823–54, vii.
Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC growth charts: United States. Adv Data. 2000;314:1–27.
Kimm SY, Barton BA, Obarzanek E, McMahon RP, Kronsberg SS, Waclawiw MA, et al. Obesity development during adolescence in a biracial cohort: the NHLBI growth and health study. Pediatrics. 2002;110:e54.
Strauss RS, Pollack HA. Epidemic increase in childhood overweight, 1986–1998. JAMA. 2001;286:2845–8.
Tauman R, O’Brien LM, Ivanenko A, Gozal D. Obesity rather than severity of sleep-disordered breathing as the major determinant of insulin resistance and altered lipidemia in snoring children. Pediatrics. 2005;116:e66–73.
Pinhas-Hamiel O, Dolan LM, Daniels SR, Standiford D, Khoury PR, Zeitler P. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996;128:608–15.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa heart study. Pediatrics. 1999;103:1175–82.
Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113:328–33.
Bendich AD, Deckelbaum RJ, editors. Can childhood obesity be prevented? Primary and secondary preventive nutrition. Totowa, NJ: Humana Press; 2001.
Richardson LP, Garrison MM, Drangsholt M, Mancl L, Leresche L. Associations between depressive symptoms and obesity during puberty. Gen Hosp Psychiatry. 2006;28:313–20.
Reilly JJ. Obesity in childhood and adolescence: evidence based clinical and public health perspectives. Postgrad Med J. 2006;82:429–37.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73.
Olszanecka-Glinianowicz M, Zahorska-Markiewicz B, Janowska J, Zurakowski A. Serum concentrations of nitric oxide, tumor necrosis factor (TNF)-alpha and TNF soluble receptors in women with overweight and obesity. Metabolism. 2004;53:1268–73.
Dixon JB, Schachter LM, O’Brien PE. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123:1134–41.
Cottam DR, Mattar SG, Barinas-Mitchell E, Eid G, Kuller L, Kelley DE, et al. The chronic inflammatory hypothesis for the morbidity associated with morbid obesity: implications and effects of weight loss. Obes Surg. 2004;14:589–600.
Kalra M, Inge T, Garcia V, Daniels S, Lawson L, Curti R, et al. Obstructive sleep apnea in extremely overweight adolescents undergoing bariatric surgery. Obes Res. 2005;13:1175–9.
Inge TH, Garcia V, Daniels S, Langford L, Kirk S, Roehrig H, et al. A multidisciplinary approach to the adolescent bariatric surgical patient. J Pediatr Surg. 2004;39:442–7; discussion 446–7.
Inge TH, Krebs NF, Garcia VF, Skelton JA, Guice KS, Strauss RS, et al. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics. 2004;114:217–23.
Rechtschaffen A, Kales A. A manual of standardized terminology. Techniques and scoring systems for sleep stages of human subjects. Los Angeles: UCLA Brain Information Service, Brain Research Institute; 1968.
American Sleep Disorders Association. EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84.
American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89.
Loredo JS, Ancoli-Israel S, Kim EJ, Lim WJ, Dimsdale JE. Effect of continuous positive airway pressure versus supplemental oxygen on sleep quality in obstructive sleep apnea: a placebo-CPAP-controlled study. Sleep. 2006;29:564–71.
Tauman R, Gulliver TE, Krishna J, Montgomery-Downs HE, O’Brien LM, Ivanenko A, et al. Persistence of obstructive sleep apnea syndrome in children after adenotonsillectomy. J Pediatr. 2006;149:803–8.
Gami AS, Caples SM, Somers VK. Obesity and obstructive sleep apnea. Endocrinol Metab Clin North Am. 2003;32:869–94.
Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90:4510–5.
Roehrs T, Zorick F, Wittig R, Conway W, Roth T. Predictors of objective level of daytime sleepiness in patients with sleep-related breathing disorders. Chest. 1989;95:1202–6.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP. Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J. 2004;25:735–41.
Somers VK. Sleep—a new cardiovascular frontier. N Engl J Med. 2005;353:2070–3.
Punjabi NM, Shahar E, Redline S, Gottlieb DJ, Givelber R, Resnick HE. Sleep-disordered breathing, glucose intolerance, and insulin resistance: the sleep heart health study. Am J Epidemiol. 2004;160:521–30.
Ziegler MG, Mills PJ, Loredo JS, Ancoli-Israel S, Dimsdale JE. Effect of continuous positive airway pressure and placebo treatment on sympathetic nervous activity in patients with obstructive sleep apnea. Chest. 2001;120:887–93.
Nelesen RA, Yu H, Ziegler MG, Mills PJ, Clausen JL, Dimsdale JE. Continuous positive airway pressure normalizes cardiac autonomic and hemodynamic responses to a laboratory stressor in apneic patients. Chest. 2001;119:1092–101.
Lattimore JD, Celermajer DS, Wilcox I. Obstructive sleep apnea and cardiovascular disease. J Am Coll Cardiol. 2003;41:1429–37.
Harsch IA, Schahin SP, Radespiel-Troger M, Weintz O, Jahreiss H, Fuchs FS, et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004;169:156–62.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalra, M., Mannaa, M., Fitz, K. et al. Effect of Surgical Weight Loss on Sleep Architecture in Adolescents with Severe Obesity. OBES SURG 18, 675–679 (2008). https://doi.org/10.1007/s11695-008-9472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9472-4