Abstract
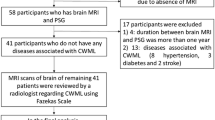
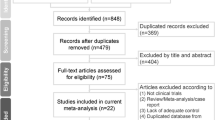
Obstructive sleep apnea (apnea) is thought to cause small vessel ischemic episodes in the brain from hypoxic events, postulated as white matter hyperintensities (hyperintensities) identified on MRI which are implicated in cognitive decline. This study sought to evaluate these correlations. A retrospective evaluation of adults who underwent polysomnography (4/1/2016 to 4/30/2017) and a brain MRI prior to apnea diagnosis or within a year post-diagnosis was completed. MRI visual evaluation of hyperintensities using Fazekas scores were collected blind to clinical data. Collated clinical/MRI data were stratified and analyzed using chi-square, fishers t-tests, ANOVA/ANCOVA and linear regression. Stratification by apnea category revealed no significant differences in any variables including hyperintensity measures (Fazekas p=0.1584; periventricular p=0.3238; deep p=0.4618; deep total p=0.1770). Stratification by Fazekas category, periventricular and deep hyperintensities revealed increasing prevalence with age (p=0.0001); however, apnea categories were not significantly associated (Fazekas p=0.1479; periventricular p=0.3188; deep p=0.4503), nor were any individual apnea indicators. Continuous apnea measurements werre not associated with any hyperintensity factor; total deep hyperintensities were not associated with any apnea factors. Continuous BMI was not found to be associated with any apnea or hyperintensity factors. Only hypertension was noted to be associated with Fazekas (p=0.0045), deep (p=0.0010) and total deep (p=0.0021) hyperintensities; however, hypertension was not associated with apnea category (p=0.3038) or any associated factors. These data suggest apneas alone from OSA are insufficient to cause WMH, but other factors appear to contribute to the complex development of small vessel ischemic injury associated with age and cognitive decline.
Similar content being viewed by others
Data availability
Data is available with an institutional data use agreement.
References
Al-Shawwa, B. A., Baadi, A. N., Goldberg, A. N. A., & Woodson, B. T. (2008). Defining common outcome metrics used in obstructive sleep apnea. Sleep Medicine Reviews, 12, 449–461
Allan, C. L., Zsoldos, E., Filippini, N., et al. (2015). Lifetime hypertension as a predictor of brain structure in older adults: cohort study with a 28-year follow-up. British Journal of Psychiatry, 206, 308–315
Avet, J., Pichot, V., Barthélémy, J. C., et al. (2014). Leukoaraiosis and ambulatory blood pressure load in a healthy elderly cohort study: the PROOF study. International Journal of Cardiology, 172, 59–63
Berry, R. B., Brooks, R., Gamaldo, C., et al. (2017). AASM scoring manual updates for 2017 (Version 2.4). Journal of Clinical Sleep Medicine, 13(5), 665–666
Bryan, R. N., Bilello, M., Davatzikos, C., et al. (2014). Effect of diabetes on brain structure: the action to control cardiovascular risk in diabetes MR imaging baseline data. Radiology, 272, 210–216
Carberry, J. C., Amatoury, J., & Eckert, D. J. (2018). Personalized management approach for OSA. Chest, 153, 744–755
Celle, S., Delon-Martin, C., Roche, F., et al. (2016). Desperately seeking grey matter volume changes in sleep apnea: A methodological review of magnetic resonance brain voxel-based morphometry studies. Sleep Medicine Reviews, 25, 112–120
Ciavarella, D., Tepedino, M., Chimenti, C., et al. (2018). Correlation between body mass index and obstructive sleep apnea severity indexes - A retrospective study. American Journal of Otolaryngology, 39, 388–391
Culebras, A. (2007). Cerebrovascular disease and the pathophysiology of obstructive sleep apnea. Current Neurology and Neuroscience Reports, 7, 173–179
DeCarli, C., Fletcher, E., Ramey, V., et al. (2005). Anatomical mapping of White Matter Hyperintensities (WMH). Stroke, 36, 50–55
Fazekas, F., Chawluk, J. B., Alavi, A., et al. (1987). MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. American Journal of Roentgenology, 149, 351–356
Gouw, A. A., van der Flier, W. M., Pantoni, L., et al. (2008). On the etiology of incident brain lacunes: longitudinal observations from the LADIS study. Stroke, 39, 3083–3085
Gray, E. L., McKenzie, D. K., & Eckert, D. J. (2017). Obstructive sleep apnea without obesity is common and difficult to treat: evidence for a distinct pathophysiological phenotype. Journal of Clinical Sleep Medicine, 15, 13
Habes, M., Sotiras, A., Erus, G., et al. (2018). White matter lesions: spatial heterogeneity, links to risk factors, cognition, genetics and atrophy. Neurology, 91, e964–e975
Halperin, J. L., Levine, G. N., Al-Khatib, S. M., et al. (2016). Further evolution of the ACC/AHA clinical practice guideline recommendation classification system: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 133, 1426–1428
Healthy Weight; Centers for Disease Control. https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html. Accessed 1 July 2017
Jehan, S., Zizi, F., Pandi-Perumal, S. R., Wall, S., et al. (2017). Obstructive sleep apnea and obesity: implications for public health. Sleep Medicine and Disorders, 1, 00019
Keenan, B. T., Kim, J., Singh, B., et al. (2018). Recognizable clinical subtypes of obstructive sleep apnea across international sleep centers: a cluster analysis. Sleep, 41, zsx214
Kepplinger, J., Barlinn, K., Boehme, A. K., et al. (2014). Association of sleep apnea with clinically silent microvascular brain tissue changes in acute cerebral ischemia. Journal of Neurology, 261, 343–349
Kern, K. C., Wright, C. B., Bergfield, K. L., et al. (2017). Blood pressure control in aging predicts cerebral atrophy related to small-vessel white matter lesions. Frontiers in Aging Neuroscience, 9, 132
Kerner, N. A., & Roose, S. P. (2016). Obstructive sleep apnea is linked to depression and cognitive impairment: evidence and potential mechanisms. The American Journal of Geriatric Psychiatry, 24, 496–508
Kim, J., Keenan, B. T., Lim, D. C., Lee, S. K., Pack, A. I., & Shin, C. (2018). Symptom-based subgroups of Koreans with obstructive sleep apnea. Journal of Clinical Sleep Medicine, 14, 437–443
Kim, K. W., MacFall, J. R., & Payne, M. E. (2008). Classification of white matter lesions on magnetic resonance imaging in elderly persons. Biological Psychiatry, 64, 273–280
Kloppenborg, R. P., Nederkoorn, P. J., Geerlings, M. I., et al. (2014). Presence and progression of white matter hyperintensities and cognition: a meta-analysis. Neurology, 82, 2127–2138
Kumar, R., Pham, T. T., Macey, P. M., et al. (2014). Abnormal myelin and axonal integrity in recently diagnosed patients with obstructive sleep apnea. Sleep, 37, 723–732
Lee, W. J., Jung, K. H., Nam, H. W., & Lee, Y. S. (2021). Effect of obstructive sleep apnea on cerebrovascular compliance and cerebral small vessel disease. PLoS One, 16, e0259469
Leppänen, T., Kulkas, A., Mervaala, E., & Töyräs, J. (2019). Increase in body mass index decreases duration of apneas and hypopneas in obstructive sleep apnea. Respiratory Care, 64, 77–84
Lin, Q., Huang, W. Q., Ma, Q. L., et al. (2017). Incidence and risk factors of leukoaraiosis from 4683 hospitalized patients: A cross-sectional study. Medicine (Baltimore), 96, e7682
Merino, J. G. (2019). White Matter hyperintensities on MRI: what is a clinician to do? Mayo Clinic Proceedings, 94, 380-382
Nishibayashi, M., Miyamoto, M., Miyamoto, T., et al. (2008). Correlation between severity of obstructive sleep apnea and prevalence of silent cerebrovascular lesions. Journal of Clinical Sleep Medicine, 4, 242–247
Nyquist, P. A., Bilgel, M. S., Gottesman, R., et al. (2014). Extreme deep white matter hyperintensity volumes are associated with African American race. Cerebrovascular Diseases, 37, 244–250
Nyquist, P. A., Bilgel, M., Gottesman, R., et al. (2015). Age differences in periventricular and deep white matter lesions. Neurobiology of Aging, 36, 1653–1658
Patel, S. K., Hanly, P. J., Smith, E. E., et al. (2015). Nocturnal hypoxemia is associated with white matter hyperintensities in patients with a minor stroke or transient ischemic attack. Journal of Clinical Sleep Medicine, 11, 1417–1424
Ryu, W. S., Woo, S. H., Schellingerhout, D., et al. (2014). Grading and interpretation of white matter hyperintensities using statistical maps. Stroke, 45, 3567–3575
Schmahmann, J. D., Smith, E. E., Eichler, F. S., et al. (2008). Cerebral white matter: neuroanatomy, clinical neurology, and neurobehavioral correlates. Annals of the New York Academy of Sciences, 1142, 266–309
Tummala, S., Palomares, J., Kang, D. W., et al. (2016). Global and regional brain non-gaussian diffusion changes in newly diagnosed patients with obstructive sleep apnea. Sleep, 39, 51–57
Wang, M., Norman, J. E., Srinivasan, V. J., et al. (2016). Metabolic, inflammatory, and microvascular determinants of white matter disease and cognitive decline. American Journal of Neurodegenerative Disease, 5, 171–177
Wardlaw, J. M., Valdés Hernández, M. C., & Muñoz-Maniega, S. (2015). What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. Journal of the American Heart Association, 4, 001140
Watson, N. F. (2016). Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. Journal of Clinical Sleep Medicine, 12, 1075–1077
Zacharias, H. U., Weihs, A., Habes, M., et al. (2021). Association between obstructive sleep apnea and brain white matter hyperintensities in a population-based Cohort in Germany. JAMA Network Open, 4(10), e2128225
Zimmerman, M. E., & Aloia, M. S. (2006). A review of neuroimaging in obstructive sleep apnea. Journal of Clinical Sleep Medicine, 2, 461–471
Zinchuk, A., & Yaggi, H. K. (2020). Phenotypic subtypes of OSA: a challenge and opportunity for precision medicine. Chest, 157, 403–420
Zinchuk, A. V., Gentry, M. J., Concato, J., & Yaggi, H. K. (2017). Phenotypes in obstructive sleep apnea: a definition, examples and evolution of approaches. Sleep Medicine Reviews, 35, 113–123
Author information
Authors and Affiliations
Contributions
Noah Schammel—data collection clinical and sleep apnea data; writing/editing.
Trevor Vandewater—data collection MRI data; writing/editing.
Stella Self—statistical analysis; writing.
Christopher Wilson—statistical analysis; writing.
Christine Schammel—project coordinator; primary writer/editor.
Ronald Cowley—project concept; editing.
Dominic Gault—project concept; writing/editing.
Lee Madeline—project concept; primary editor.
Corresponding author
Ethics declarations
Declarations of conflicts of interest
All authors declare they have no financial or non-financial conflicts of interest.
Ethics approval
The submitted work is original and has not been published elsewhere in any form or language.
Consent to participate
This project was approved by the Prisma Health/SC IRB prior to initiation. A universal consent was used for data collection and all data was de-identified.
Consent to publish
not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 43.2 KB)
Rights and permissions
About this article
Cite this article
Schammel, N.C., VandeWater, T., Self, S. et al. Obstructive sleep apnea and white matter hyperintensities: correlation or causation?. Brain Imaging and Behavior 16, 1671–1683 (2022). https://doi.org/10.1007/s11682-022-00642-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-022-00642-9