Abstract
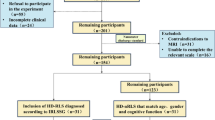
Hemodialysis with restless legs syndrome (HD-RLS) is associated with alterations in neuronal function, the blood-brain barrier and iron deposition, thus affecting cerebral metabolism and perfusion. This study utilized three-dimensional arterial spin labeling (ASL) to identify HD-RLS-related perfusion patterns and potential relationships with disease severity. Twenty-six HD-RLS patients, 30 hemodialysis patients without restless legs syndrome (HD-nRLS) and 30 age-, sex-, and education-matched healthy controls were included in this study. One-way analysis of covariance and post hoc analyses were used to assess differences in cerebral blood flow (CBF) values, demographics and clinical data among the three groups. Pearson’s correlation analysis was conducted between altered CBF values in the HD-RLS group and clinical data. Compared with HD-nRLS patients, HD-RLS patients showed increased CBF in the right primary motor cortex (false discovery rate [FDR]-corrected P < 0.05). Compared with the normal controls, both HD subgroups (i.e., those with and without RLS) exhibited consistent CBF changes, including increased CBF in the left medial superior frontal gyrus and bilateral thalamus and decreased CBF in the left insular cortices (FDR-corrected P < 0.05). This abnormal hyperperfusion in the sensorimotor cortex and basal ganglia provides evidence for a sensory processing disorder in RLS that may be involved in the pathogenesis of RLS in HD patients.


Similar content being viewed by others
References
Allen, R. P., Picchietti, D., Hening, W. A., Trenkwalder, C., Walters, A. S., Montplaisi, J., Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health, & International Restless Legs Syndrome Study Group. (2003). Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine, 4, 101–119.
Allen, R. P., Picchietti, D. L., Garcia-Borreguero, D., Ondo, W. G., Walters, A. S., Winkelman, J. W., Zucconi, M., Ferri, R., Trenkwalder, C., Lee, H. B., & International Restless Legs Syndrome Study Group. (2014). Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: Updated international restless legs syndrome study group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Medicine, 15, 860–873.
Araujo, S. M., de Bruin, V. M., Nepomuceno, L. A., Maximo, M. L., Daher Ede, F., Correia Ferrer, D. P., & de Bruin, P. F. (2010). Restless legs syndrome in end-stage renal disease: Clinical characteristics and associated comorbidities. Sleep Medicine, 11, 785–790.
Aslan, S., & Lu, H. (2010). On the sensitivity of ASL MRI in detecting regional differences in cerebral blood flow. Magnetic Resonance Imaging, 28, 928–935.
Buhmann, C., Glauche, V., Stürenburg, H. J., Oechsner, M., Weiller, C., & Büchel, C. (2003). Pharmacologically modulated fMRI--cortical responsiveness to levodopa in drug-naive hemiparkinsonian patients. Brain., 126, 451–461.
Cervenka, S., Pålhagen, S. E., Comley, R. A., Panagiotidis, G., Cselényi, Z., Matthews, J. C., Lai, R. Y., Halldin, C., & Farde, L. (2006). Support for dopaminergic hypoactivity in restless legs syndrome: A PET study on D2-receptor binding. Brain., 129, 2017–2028.
Chai, C., Wang, H., Liu, S., Chu, Z. Q., Li, J., Qian, T., Haacke, E. M., Xia, S., & Shen, W. (2019). Increased iron deposition of deep cerebral gray matter structures in hemodialysis patients: A longitudinal study using quantitative susceptibility mapping. Journal of Magnetic Resonance Imaging, 49, 786–799.
Cheng, B. C., Chen, P. C., Chen, P. C., Lu, C. H., Huang, Y. C., Chou, K. H., Li, S. H., Lin, A. N., & Lin, W. C. (2019). Decreased cerebral blood flow and improved cognitive function in patients with end-stage renal disease after peritoneal dialysis: An arterial spin-labelling study. European Radiology, 29, 1415–1424.
De Vis, J. B., et al. (2018). Arterial-spin-labeling (ASL) perfusion MRI predicts cognitive function in elderly individuals: A 4-year longitudinal study. Journal of Magnetic Resonance Imaging, 48, 449–458.
Ding, D., Li, P., Ma, X. Y., Dun, W. H., Yang, S. F., Ma, S. H., Liu, H. J., & Zhang, M. (2018). The relationship between putamen-SMA functional connectivity and sensorimotor abnormality in ESRD patients. Brain Imaging and Behavior, 12, 1346–1354.
Earley, C. J., Connor, J. R., Beard, J. L., Malecki, E. A., Epstein, D. K., & Allen, R. P. (2000). Abnormalities in CSF concentrations of ferritin and transferrin in restless legs syndrome. Neurology., 54, 1698–1700.
Earley, C. J., Connor, J., Garcia-Borreguero, D., Jenner, P., Winkelman, J., Zee, P. C., & Allen, R. (2014). Altered brain iron homeostasis and dopaminergic function in restless legs syndrome (Willis-Ekbom disease). Sleep Medicine, 15, 1288–1301.
Earley, C. J., Uhl, G. R., Clemens, S., & Ferré, S. (2017). Connectome and molecular pharmacological differences in the dopaminergic system in restless legs syndrome (RLS): Plastic changes and neuroadaptations that may contribute to augmentation. Sleep Medicine, 31, 71–77.
Fornito, A., Zalesky, A., & Breakspear, M. (2015). The connectomics of brain disorders. Nature Reviews. Neuroscience, 16, 159–172.
Graziano, M. S., Taylor, C. S., Moore, T., & Cooke, D. F. (2002). The cortical control of movement revisited. Neuron., 36, 349–362.
Jiang, X. L., Wen, J. Q., Zhang, L. J., Zheng, G., Li, X., Zhang, Z., Liu, Y., Zheng, L. J., Wu, L., Chen, H. J., Kong, X., Luo, S., Lu, G. M., Ji, X. M., & Zhang, Z. J. (2016). Cerebral blood flow changes in hemodialysis and peritoneal dialysis patients: An arterial-spin labeling MR imaging. Metabolic Brain Disease, 31, 929–936.
Ku, J., Cho, Y. W., Lee, Y. S., Moon, H. J., Chang, H., Earley, C. J., & Allen, R. P. (2014). Functional connectivity alternation of the thalamus in restless legs syndrome patients during the asymptomatic period: A resting-state connectivity study using functional magnetic resonance imaging. Sleep Medicine, 15, 289–294.
Ku, J., Lee, Y. S., Chang, H. W., Earley, C. J., Allen, R. P., & Cho, Y. W. (2018). Diurnal variation of default mode network in patients with restless legs syndrome. Sleep Medicine, 41, 1–8.
Kumakura, Y., Gjedde, A., Danielsen, E. H., Christensen, S., & Cumming, P. (2006). Dopamine storage capacity in caudate and putamen of patients with early Parkinson's disease: Correlation with asymmetry of motor symptoms. Journal of Cerebral Blood Flow and Metabolism, 26, 358–370.
Lee, S. J., Kim, J. S., Song, I. U., An, J. Y., Kim, Y. I., & Lee, K. S. (2009). Poststroke restless legs syndrome and lesion location: Anatomical considerations. Movement Disorders, 24, 77–84.
Li, P., Ding, D., Ma, X. Y., Zhang, H. W., Liu, J. X., & Zhang, M. (2018). Altered intrinsic brain activity and memory performance improvement in patients with end-stage renal disease during a single dialysis session. Brain Imaging and Behavior, 12, 1640–1649.
Lin, C. H., Wu, V. C., Li, W. Y., Sy, H. N., Wu, S. L., Chang, C. C., Chiu, P. F., Lion, H. H., Lin, C. Y., Chang, H. W., Lin, S. Y., Wu, K. D., Chen, Y. M., & Wu, R. M. (2013). Restless legs syndrome in end-stage renal disease: A multicenter study in Taiwan. European Journal of Neurology, 20, 1025–1031.
Liu, C., Dai, Z., Zhang, R., Zhang, M., Hou, Y., Qi, Z., Huang, Z., Lin, Y., Zhan, S., He, Y., & Wang, Y. (2015). Mapping intrinsic functional brain changes and repetitive transcranial magnetic stimulation neuromodulation in idiopathic restless legs syndrome: A resting-state functional magnetic resonance imaging study. Sleep Medicine, 16, 785–791.
Mattson, M. P., & Shea, T. B. (2003). Folate and homocysteine metabolism in neural plasticity and neurodegenerative disorders. Trends in Neurosciences, 26, 137–146.
Meguid El Nahas, A., & Bello, A. K. (2005). Chronic kidney disease: The global challenge. Lancet., 365, 331–340.
Meier, J. D., et al. (2008). Complex organization of human primary motor cortex: A high-resolution fMRI study. Journal of Neurophysiology, 100, 1800–1812.
Mu, J., et al. (2018). The variation of motor-related brain structure and its relation to abnormal motor behaviors in end-stage renal disease patients with restless legs syndrome. Brain Imaging and Behavior.
Novak, M., Winkelman, J. W., & Unruh, M. (2015). Restless legs syndrome in patients with chronic kidney disease. Seminars in Nephrology, 35, 347–358.
Rizzo, G., Li, X., Galantucci, S., Filippi, M., & Cho, Y. W. (2017). Brain imaging and networks in restless legs syndrome. Sleep Medicine, 31, 39–48.
San Pedro, E. C., Mountz, J. M., Mountz, J. D., Liu, H. G., Katholi, C. R., & Deutsch, G. (1998). Familial painful restless legs syndrome correlates with pain dependent variation of blood flow to the caudate, thalamus, and anterior cingulate gyrus. The Journal of Rheumatology, 25, 2270–2275.
Schneider, S., et al. (2012). Cognitive function at 2443 mumol/l creatinine. BMC Nephrology, 13, 86.
Sloand, J. A., Shelly, M. A., Feigin, A., Bernstein, P., & Monk, R. D. (2004). A double-blind, placebo-controlled trial of intravenous iron dextran therapy in patients with ESRD and restless legs syndrome. American Journal of Kidney Diseases, 43, 663–670.
Stefanidis, I., Vainas, A., Giannaki, C. D., Dardiotis, E., Spanoulis, A., Sounidaki, M., Eleftheriadis, T., Liakopoulos, V., Karatzaferi, C., Sakkas, G. K., Zintzaras, E., & Hadjigeorgiou, G. M. (2015). Restless legs syndrome does not affect 3-year mortality in hemodialysis patients. Sleep Medicine, 16, 1131–1138.
Szentkiralyi, A., et al. (2014). Multimorbidity and the risk of restless legs syndrome in 2 prospective cohort studies. Neurology., 82, 2026–2033.
Takaki, J., Nishi, T., Nangaku, M., Shimoyama, H., Inada, T., Matsuyama, N., Kumano, H., & Kuboki, T. (2003). Clinical and psychological aspects of restless legs syndrome in uremic patients on hemodialysis. American Journal of Kidney Diseases, 41, 833–839.
Tessitore, A., Esposito, F., Monsurrò, M. R., Graziano, S., Panza, D., Russo, A., Migliaccio, R., Conforti, F. L., Morrone, R., Quattrone, A., di Salle, F., & Tedeschi, G. (2006). Subcortical motor plasticity in patients with sporadic ALS: An fMRI study. Brain Research Bulletin, 69, 489–494.
Trenkwalder, C., Paulus, W., & Walters, A. S. (2005). The restless legs syndrome. Lancet Neurology, 4, 465–475.
Ulfberg, J., Nyström, B., Carter, N., & Edling, C. (2001). Prevalence of restless legs syndrome among men aged 18 to 64 years: An association with somatic disease and neuropsychiatric symptoms. Movement Disorders, 16, 1159–1163.
Wenderoth, N., Debaere, F., Sunaert, S., & Swinnen, S. P. (2005). The role of anterior cingulate cortex and precuneus in the coordination of motor behaviour. The European Journal of Neuroscience, 22, 235–246.
Xu, G., Rowley, H. A., Wu, G., Alsop, D. C., Shankaranarayanan, A., Dowling, M., Christian, B. T., Oakes, T. R., & Johnson, S. C. (2010). Reliability and precision of pseudo-continuous arterial spin labeling perfusion MRI on 3.0 T and comparison with 15O-water PET in elderly subjects at risk for Alzheimer's disease. NMR in Biomedicine, 23, 286–293.
Yang, F. C., et al. (2018). Altered brain functional Connectome in migraine with and without restless legs syndrome: A resting-state functional MRI study. Frontiers in Neurology, 9, 25.
Zhang, S., & Li, C. S. (2012). Functional connectivity mapping of the human precuneus by resting state fMRI. Neuroimage., 59, 3548–3562.
Zhuo, Y., Wu, Y., Xu, Y., Lu, L., Li, T., Wang, X., & Li, K. (2017). Combined resting state functional magnetic resonance imaging and diffusion tensor imaging study in patients with idiopathic restless legs syndrome. Sleep Medicine, 38, 96–103.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interests
The authors declare that there are no potential conflicts of interest regarding the publication of this paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, H., Han, X., Jin, M. et al. Cerebral blood flow alterations in hemodialysis patients with and without restless legs syndrome: an arterial spin labeling study. Brain Imaging and Behavior 15, 401–409 (2021). https://doi.org/10.1007/s11682-020-00268-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-020-00268-9