Abstract
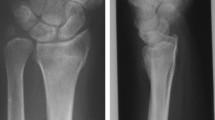
In operations of palmar dislocated distal radius fractures, the palmar locking plate has already proved itself early. The principle of “angle stability” works as an internal fixator and a stable support of the joint area makes it possible without danger of secondary dislocation. This is an advantage particularly for older patients with poor bone quality.
However, with the palmar locking plate there are also limits and the indication has to be evaluated individually. The correct placement of the screws is particularly important. An intraarticular placement of the screws is described in1–3% of the cases. Special intraoperative X-rays can protect against this.
A rupture of the EPL tendon is described in 0–3% of cases. A2, A3, C1 and C2 fractures according to the AO classification are favorable for this method. Here the fracture line can be reconstructed anatomically and the joint fragments supported sufficiently by the plate. More distally placed palmar fragments can further be held with multidirectionally locking plates. With the C3 fracture (AO) the palmar locking plate is pushed to its limits. Defect replenishment or even many different osteosyntheses are also frequently necessary here.
Zusammenfassung
Bei Operation der palmar dislozierten distalen Radiusfraktur hat sich die palmare Plattenosteosynthese schon früh bewährt. Das Prinzip der „Winkelstabilität“ wirkt wie ein Fixateur interne und ermöglicht so von Anfang an eine stabile Abstützung der Gelenkfläche ohne Gefahr der sekundären Dislokation. Dies ist besonders für ältere Patienten mit schlechter Knochenqualität von Vorteil.
Auch bei der palmaren winkelstabilen Platte gibt es Grenzen und muss deren Indikation individuell gestellt werden. Besonders wichtig ist die korrekte Platzierung der Schrauben. Eine intraartikuläre Fehlplatzierung ist in immerhin 1–3% der Fälle beschrieben und kann durch intraoperative spezielle Röntgenkontrolle vermieden werden. Eine daraus resultierende Ruptur der EPL-Sehne wird in 0–3% beschrieben. In der Literatur werden als für dieses Verfahren günstige Frakturen die A2, A3, C1, C2-Frakturen nach AO mit ausreichend großem metaphysären Fragment angesehen. Hier können die Frakturlinie durch die Platte überbrückt und die Gelenkfragmente ausreichend abgestützt werden. Weiter distale palmare Fragmente können mit multidirektionalen winkelstabilen Platten gut gefasst werden. Bei der C3-Fraktur stößt die palmare winkelstabile Platte an ihre Grenzen. Häufig wird hier zusätzlich eine Defektauffüllung oder sogar eine Mehrfachosteosynthese notwendig.
Similar content being viewed by others
Referenzen
Anand A, Sood LK, Sud A, Singh T, Kamojia R (2004) Role of dynamic external fixator in the management of fractures of distal end of radius. J Indian Med Assoc 102(9):495–496; 498–499
Al Rashid M, Theivendran K, Craigen MA (2006) Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg Br 88(12):1610–1612
Arora R, Lutz M, Hemmerbicher A, Kappinger D, Espen D, Gabl M (2007) Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma 21(5):316–322
Fernandez DL, Orbay JL (2004) Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg (Am) 29(1):96–102
Gartland JJ, Werley CW (1951) Evaluation of healed Coles fractures. J Bone Joint Surg Am 33:895–907
Hove LM (1994) Delayed rupture of the thumb extensor tendon.A 5-year study of 18 consecutive cases. Acta Orthop Scand 65(2):199–203
Handoll HH, Madhok R (2003) From evidence to best practice in the management of fractures of the distal radius in adults: working towards a research agenda. BMC Musculoskelet Disord 27(4):27
Hunsaker FG, Cioffi DA, Amadio PC, Wright JG, Caughlin B (2002) The American academy of orthopaedic surgeon's outcomes instruments: normative values from the general population. J Bone Joint Surg Am 84-A(2):208–215
Jakim I, Pieterse HS, Sweat MB (1991) External fixation for intra-articular fractures of the distal radius. J Bone Joint Surg Br 73(2):302–306
Kamano M, Koshimmune M, Kazuki Y, Honda Y (2005) Palmar plating system for Colles' fractures – a preliminary report. J Hand Surg (Am) 30(4):750–755
Koshimmune M, Kamano M, Takamabu K, Ohashi H (2005) A randomized comparison of locking and non-locking palmar plating for unstable Colles' fractures in the elderly. J Hand Surg (Br) 30(5):499–503
Kreder HJ, Agel J, Mc Kee MD, Schemitsch EH, Stephen D, Hanel DP (2006) A randomized,controlled trial of distal radius fractures with metaphyseal displacement but without joint incongruity: closed reduction and casting versus closed reduction, spanning external fixation, and optional percutaneous K-wires. J Orthop Trauma 20(2):115–121
Lee HC, Wong YS, Chan BK, Low CO (2003) Fixation of distal radius fractures using AO titanium volar distal radius plate. Hand Surg 8(1):7–15
Leung F, Zhu L, Ho H, Lu WW, Chow SP (2003) Palmar plate fixation of AO type C2. fracture of distal radius using a locking compression plate–a biomechanical study in a cadaveric model. J Hand Surg (Br) 28(3):263–266
Margaliot Z, Haase SC, Kotsis SV, Ku HM, Chung KC (2005) A meta-analysis of outcomes of external fixation versus plate osteosynthesis for unstable distal radius fractures. J Hand Surg (Am) 30(6):1185–1199 (Review)
Martini AK (1999) Bewertungsschemata zur Beurteilung des Handgelenkes. Handchir Mikrochir Plast Chir 31:153–154
Mec Dermid JC, Fess EE, Bell-Krotoski J, Santore G (2002) A research agenda for hand therapy. J Hand Ther 15(1):3–15
Nana AD, Joshi A, Lichtman DM (2005) Plating of the distal radius. J Am Acad Orthop Surg 13(3):159–171
Orbay JL, Fernandez DL (2002) Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg (Am) 27(2):205–215
Osada D, Viegas SF, Shah MA, Morris RP, Patterson RM (2003) Comparison of different distal radius dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg (Am) 28(1):94–104
Ring D, Jupiter JB (2005) Treatment of osteoporotic distal radius fractures. Osteoporos Int 16(Suppl 2):S80–S84
Rommens PM, Broos PL (1992) External fixation of the distal end of the radius: the same technique for different patient populations? Arch Orthop Trauma Surg 111(3):165–170
Sakhaii M, Groenewold U, Klonz A, Reilmann H (2003) Results after palmar plate-osteosynthesis with angularly stable T-plate in 100 distal radius fractures: a prospective study. Unfallchirurg 106(4):272–280
Schmelzer-Schmied N, Schröder K, Wieloch P, Martini AK, Daecke W (2007) Ergebnisse nach operativer Versorgung der distalen Radiusfraktur des älteren Patienten. Obere Extremität 2:13–18
Siebert HR, Klonz A (2005) Distale Radiusfraktur. Unfallchirurg 108:135–153
Thielke KH, Wagner T, Bartsch S, Echtermeyer V (2003) Angularly stable radius plate: progress in treatment of problematic distal radius fracture? Chirurg 74(11):1057–1063
Walz M, Kolbow B, Auerbach F (2004) Do fixed-angle T-plates offer advantages for distal radius fractures in elderly patients? Unfallchirurg 107(8):664–646; 668–670
Westphal T, Piatek S, Schubert S,Winckler S (2005) Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg 125(8):507–514
Wright TW, Horodyski M, Smith DW (2005) Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg (Am) 30(2):289–299
Yen S, Hwang CY, Hwang MH (1991) A semiinvasive method for articular Colles' fractures. Clin Orthop Relat Res 263:154–164
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmelzer-Schmied, N., Martini, A.K. & Jung, M. Die palmare winkelstabile Plattenosteosynthese bei distaler Radiusfraktur. Obere Extremität 2, 150–155 (2007). https://doi.org/10.1007/s11678-007-0048-z
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s11678-007-0048-z
Key words
- distal radius fracture
- locking plate
- internal fixator
- external fixator
- tendon rupture
- defect replenishment