Abstract
Summary
In a community-dwelling elderly cohort, dysmobility syndrome was associated with elevated odds of morphometric vertebral fracture or any prevalent fracture, independent of age and covariates. Dysmobility syndrome improved discrimination for fracture when added to the FRAX score.
Introduction
Dysmobility syndrome was coined to indicate patients with impaired musculoskeletal health. Data on the association of dysmobility syndrome with prevalent morphometric vertebral fracture (VF) in elderly persons are limited.
Methods
A total of 1369 community-dwelling elderly subjects (mean age 71.6 years; women 66%) were analyzed. Dysmobility syndrome was defined as ≥ 3 components among falls, low lean mass, high fat mass, osteoporosis, low grip strength, and low timed get-up-and-go performance. VF was defined as a ≥ 25% reduction in the height of vertebral bodies in plain radiographs. Modified cutpoints of each component at which elevate the odds of fracture were investigated using receiver-operating characteristics analysis. Net reclassification improvement (NRI) and integrated discrimination index (IDI) were calculated to assess additive discriminatory value of dysmobility syndrome over FRAX.
Results
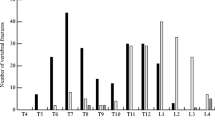
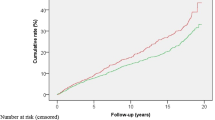
The prevalence of VF and any fracture composite of VF and non-VF was 16% and 25%, respectively, increasing according to number of dysmobility components (from 0 to 5; VF 10–35%; any fracture 16–45%). Dysmobility syndrome was associated with elevated odds of VF (adjusted OR [aOR] 1.52, 95% CI 1.08–2.15) or any fracture (aOR 1.46, 95% CI 1.07–1.98) but no longer with non-VF (aOR 1.31, 95% CI 0.86–1.98) in multivariate model, whereas modified definition showed robust association with non-VF (aOR 1.79, 95% CI 1.23–2.60). Dysmobility syndrome improved discrimination for prevalent fracture when added to FRAX (NRI 0.25, 95% CI 0.13–0.37; IDI 0.020, 95% CI 0.014–0.026).
Conclusions
Dysmobility syndrome was associated with elevated odds of morphometric VF in community-dwelling older adults, independent of age and covariates.

Similar content being viewed by others
References
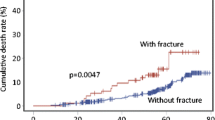
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 159:1215–1220
Tran T, Bliuc D, van Geel T, Adachi JD, Berger C, van den Bergh J, Eisman JA, Geusens P, Goltzman D, Hanley DA, Josse RG, Kaiser SM, Kovacs CS, Langsetmo L, Prior JC, Nguyen TV, Center JR (2017) Population-wide impact of non-hip non-vertebral fractures on mortality. J Bone Miner Res 32:1802–1810
Binkley N, Blank RD, Leslie WD, Lewiecki EM, Eisman JA, Bilezikian JP (2017) Osteoporosis in crisis: it’s time to focus on fracture. J Bone Miner Res 32:1391–1394
Binkley N, Krueger D, Buehring B (2013) What’s in a name revisited: should osteoporosis and sarcopenia be considered components of “dysmobility syndrome?”. Osteoporos Int 24:2955–2959
Looker AC (2015) Dysmobility syndrome and mortality risk in US men and women age 50 years and older. Osteoporos Int 26:93–102
Lee WJ, Liu LK, Hwang AC, Peng LN, Lin MH, Chen LK (2017) Dysmobility syndrome and risk of mortality for community-dwelling middle-aged and older adults: the nexus of aging and body composition. Sci Rep 7:8785
Iolascon G, Moretti A, Giamattei MT, Migliaccio S, Gimigliano F (2015) Prevalent fragility fractures as risk factor for skeletal muscle function deficit and dysmobility syndrome in post-menopausal women. Aging Clin Exp Res 27(Suppl 1):S11–S16
Buehring B, Hansen KE, Lewis BL, Cummings SR, Lane NE, Binkley N, et al (2018) Dysmobility syndrome independently increases fracture risk in the osteoporotic fractures in men (MrOS) prospective cohort study. J Bone Miner Res. https://doi.org/10.1002/jbmr.3455
Kendler DL, Bauer DC, Davison KS, Dian L, Hanley DA, Harris ST et al (2016) Vertebral fractures: clinical importance and management. Am J Med 129(221):e221–e210
Lee EY, Kim HC, Rhee Y, Youm Y, Kim KM, Lee JM, Choi DP, Yun YM, Kim CO (2014) The Korean urban rural elderly cohort study: study design and protocol. BMC Geriatr 14:33
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis: The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Lee EY, Lee SJ, Kim KM, Seo DH, Lee SW, Choi HS, Kim HC, Youm Y, Kim CO, Rhee Y (2017) Lower jump power rather than muscle mass itself is associated with vertebral fracture in community-dwelling elderly Korean women. Calcif Tissue Int 100:585–594
Duboeuf F, Bauer DC, Chapurlat RD, Dinten JM, Delmas P (2005) Assessment of vertebral fracture using densitometric morphometry. J Clin Densitom 8:362–368
Hong N, Kim CO, Youm Y, Kim HC, Rhee Y (2018) Low peak jump power is associated with elevated odds of dysmobility syndrome in community-dwelling elderly individuals: the Korean Urban Rural Elderly (KURE) study. Osteoporos Int 29:1427–1436. https://doi.org/10.1007/s00198-018-4466-0
Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M et al (2003) Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing 32:315–320
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JSW, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56:M366–M372
Chun MY (2012) Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med 33:144–151
O’Bryant SE, Humphreys JD, Smith GE, Ivnik RJ, Graff-Radford NR, Petersen RC et al (2008) Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol 65:963–967
Anonymous (1968) Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser 405:5–37
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Pencina MJ, Steyerberg EW, D’Agostino RB (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30:11–21
Clynes MA, Edwards MH, Buehring B, Dennison EM, Binkley N, Cooper C (2015) Definitions of sarcopenia: associations with previous falls and fracture in a population sample. Calcif Tissue Int 97:445–452
Hill KD, Farrier K, Russell M, Burton E (2017) Dysmobility syndrome: current perspectives. Clin Interv Aging 12:145–152
Braun BL, Gerberich SG, Sidney S (1994) Injury events: utility of self report in retrospective identification in the USA. J Epidemiol Community Health 48:604–605
Johansson H, Oden A, McCloskey EV, Kanis JA (2014) Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos Int 25:235–241
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20:1813–1819
Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34:195–202
Nguyen TV (2018) Individualized fracture risk assessment: state-of-the-art and room for improvement. Osteoporosis and Sarcopenia 4:2–10
Fleming J, Matthews FE, Brayne C, Cambridge City over-75s Cohort study c (2008) Falls in advanced old age: recalled falls and prospective follow-up of over-90-year-olds in the Cambridge City over-75s Cohort study. BMC Geriatr 8:6
Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG, Mathews M, Barron JR, Fitzpatrick DG, Gulliver W, Zhang H (2005) Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr 81:74–78
Acknowledgements
We thank all our participants and the technical staff of the KURE study.
Funding
This study was funded by the Research of Korea Centers for Disease Control and Prevention (2013-E63007-01, 2013-E63007-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Institutional Review Board (IRB) of Severance Hospital (IRB no. 4-2012-0172), with written informed consent obtained from all participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the IRB and with the 1964 Helsinki Declaration and its later amendments.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Hong, N., Kim, C.O., Youm, Y. et al. Dysmobility syndrome is associated with prevalent morphometric vertebral fracture in older adults: the Korean Urban-Rural Elderly (KURE) study. Arch Osteoporos 13, 86 (2018). https://doi.org/10.1007/s11657-018-0500-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0500-2