Abstract
Objective
To investigate the molecular mechanisms underlying the beneficial effect of electroacupuncture (EA) in experimental models of Alzheimer’s disease (AD) in vivo.
Methods
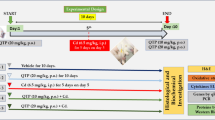
Senescence-accelerated mouse prone 8 (SAMP8) mice were used as AD models and received EA at Yingxiang (LI 20, bilateral) and Yintang (GV 29) points for 20 days. For certain experiments, SAMP8 mice were injected intravenously with human fibrin (2 mg). The Morris water maze test was used to assess cognitive and memory abilities. The changes of tight junctions of blood-brain barrier (BBB) in mice were observed by transmission electron microscope. The expressions of fibrin, amyloid- β (Aβ), and ionized calcium-binding adapter molecule 1 (IBa-1) in mouse hippocampus (CA1/CA3) were detected by reverse transcription-quantitative polymerase chain reaction (qRT-PCR), Western blot or immunohistochemical staining. The expression of fibrin in mouse plasma was detected by enzyme-linked immunosorbent assay. The expressions of tight junction proteins zonula occludens-1 and claudin-5 in hippocampus were detected by qRT-PCR and immunofluorescence staining. Apoptosis of hippocampal neurons was detected by terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) staining.
Results
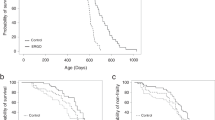
Fibrin was time-dependently deposited in the hippocampus of SAMP8 mice and this was inhibited by EA treatment (P<0.05 or P<0.01). Furthermore, EA treatment suppressed the accumulation of Aβ in the hippocampus of SAMP8 mice (P<0.01), which was reversed by fibrin injection (P<0.05 or P<0.01). EA improved SAMP8 mice cognitive impairment and BBB permeability (P<0.05 or P<0.01). Moreover, EA decreased reactive oxygen species levels and neuroinflammation in the hippocampus of SAMP8 mice, which was reversed by fibrin injection (P<0.05 or P<0.01). Mechanistically, EA inhibited the promoting effect of fibrin on the high mobility group box protein 1 (HMGB1)/toll-like receptor 4 (TLR4) and receptor for advanced glycation end products (RAGE)/nicotinamide adenine dinucleotide phosphate (NADPH) signaling pathways (P<0.01).
Conclusion
EA may potentially improve cognitive impairment in AD via inhibition of fibrin/A β deposition and deactivation of the HMGB1/TLR4 and RAGE/NADPH signaling pathways.
Similar content being viewed by others
References
Soria Lopez JA, González HM, Léger GC. Alzheimer’s disease. Handb Clin Neurol 2019;167:231–255.
Eratne D, Loi SM. Alzheimer’s disease: clinical update on epidemiology, pathophysiology and diagnosis. Australas Psychiatry 2018;26:347–357.
Oboudiyat C, Glazer H, Seifan A, Greer C, Isaacson RS. Alzheimer’s disease. Semin Neurol 2013;33:313–329.
Pinheiro L, Faustino C. Therapeutic strategies targeting amyloid- β in Alzheimer’s disease. Curr Alzheimer Res 2019;16:418–452.
Ashrafian H, Zadeh EH, Khan RH. Review on Alzheimer’s disease: inhibition of amyloid beta and tau tangle formation. Int J Biol Macromol 2021;167:382–394.
Dubois B, Villain N, Frisoni GB, Rabinovici GD, Sabbagh M, Cappa S, et al. Clinical diagnosis of Alzheimer’s disease: recommendations of the International Working Group. Lancet Neurol 2021;20:484–496.
Lane CA, Hardy J, Schott JM. Alzheimer’s disease. Eur J Neurol 2018;25:59–70.
Weisel JW. Fibrinogen and fibrin. Adv Protein Chem 2005;70:247–299.
Petersen MA, Ryu JK, Akassoglou K. Fibrinogen in neurological diseases: mechanisms, imaging and therapeutics. Nat Rev Neurosci 2018;19:283–301.
Cortes-Canteli M, Mattei L, Richards AT, Norris EH, Strickland S. Fibrin deposited in the Alzheimer’s disease brain promotes neuronal degeneration. Neurobiol Aging 2015;36:608–617.
Cortes-Canteli M, Zamolodchikov D, Ahn HJ, Strickland S, Norris EH. Fibrinogen and altered hemostasis in Alzheimer’s disease. J Alzheimer Dis 2012;32:599–608.
Cai M, Lee JH, Yang EJ. Electroacupuncture attenuates cognition impairment via anti-neuroinflammation in an Alzheimer’s disease animal model. J Neuroinflammation 2019;16:264.
Jiang YH, He JK, Li R, Chen ZH, Jia BH. Mechanisms of Acupuncture in improving Alzheimer’s disease caused by mitochondrial damage. Chin J Integr Med 2022;28:272–280.
Chen B, Lin WQ, Li ZF, Zhong XY, Wang J, You XF, et al. Electroacupuncture attenuates ischemic brain injury and cellular apoptosis via mitochondrial translocation of cofilin. Chin J Integr Med 2021;27:705–712.
Aldad TS, Gan G, Gao XB, Taylor HS. Fetal radiofrequency radiation exposure from 800–1900 mhz-rated cellular telephones affects neurodevelopment and behavior in mice. Sci Rep 2012;2:312.
Thal DR, Walter J, Saido TC, Fändrich M. Neuropathology and biochemistry of Aβ and its aggregates in Alzheimer’s disease. Acta Neuropathol 2015;129:167–182.
Ma Q, Zhao Z, Sagare AP, Wu Y, Wang M, Owens NC, et al. Blood-brain barrier-associated pericytes internalize and clear aggregated amyloid-β 42 by LRP1-dependent apolipoprotein E isoform-specific mechanism. Mol Neurodegener 2018;13:57.
Zhu L, Li R. Blood-brain barrier permeable chitosan oligosaccharides interfere with β -amyloid aggregation and alleviate β -amyloid protein mediated neurotoxicity and neuroinflammation in a dose- and degree of polymerization-dependent manner. Mar Drugs 2020;18:488.
Daneman R, Prat A. The blood-brain barrier. Cold Spring Harb Perspect Biol 2015;7:a020412.
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis 2010;37:13–25.
Cai Z, Qiao PF, Wan CQ, Cai M, Zhou NK, Li Q. Role of blood-brain barrier in Alzheimer’s disease. J Alzheimer Dis 2018;63:1223–1234.
Sweeney MD, Sagare AP, Zlokovic BV. Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol 2018;14:133–150.
Baulch JE, Acharya MM, Agrawal S, Apodaca LA, Monteiro C, Agrawal A. Immune and inflammatory determinants underlying Alzheimer’s disease pathology. J Neuroimmune Pharmacol 2020;15:852–862.
Di Bona D, Scapagnini G, Candore G, Castiglia L, Colonna-Romano G, Duro G, et al. Immune-inflammatory responses and oxidative stress in Alzheimer’s disease: therapeutic implications. Curr Pharm Des 2010;16:684–691.
Hansen DV, Hanson JE, Sheng M. Microglia in Alzheimer’s disease. J Cell Biol 2018;217:459–472.
Zhou Y, Song WM, Andhey PS, Swain A, Levy T, Miller KR, et al. Human and mouse single-nucleus transcriptomics reveal TREM2-dependent and TREM2-independent cellular responses in Alzheimer’s disease. Nat Med 2020;26:131–142.
Kwon HS, Koh SH. Neuroinflammation in neurodegenerative disorders: the roles of microglia and astrocytes. Transl Neurodegener 2020;9:42.
Cai Z, Hussain MD, Yan LJ. Microglia, neuroinflammation, and beta-amyloid protein in Alzheimer’s disease. Int J Neurosci 2014;124:307–321.
Kaur D, Sharma V, Deshmukh R. Activation of microglia and astrocytes: a roadway to neuroinflammation and Alzheimer’s disease. Inflammopharmacology 2019;27:663–677.
Iba T, Nakarai E, Takayama T, Nakajima K, Sasaoka T, Ohno Y. Combination effect of antithrombin and recombinant human soluble thrombomodulin in a lipopolysaccharide induced rat sepsis model. Crit Care 2009;13:R203.
Nakamura T, Okui T, Hasegawa K, Ryumon S, Ibaragi S, Ono K, et al. High mobility group box 1 induces bone pain associated with bone invasion in a mouse model of advanced head and neck cancer. Oncol Rep 2020;44:2547–2558.
Xu X, Piao HN, Aosai F, Zeng XY, Cheng JH, Cui YX, et al. Arctigenin protects against depression by inhibiting microglial activation and neuroinflammation via HMGB1/TLR4/NF- κ B and TNF- α/TNFR1/NF- κ B pathways. Br J Pharmacol 2020;177:5224–5245.
Wang J, Li R, Peng Z, Hu B, Rao X, Li J. HMGB1 participates in LPS-induced acute lung injury by activating the AIM2 inflammasome in macrophages and inducing polarization of M1 macrophages via TLR2, TLR4, and RAGE/NF- κ B signaling pathways. Int J Mol Med 2020;45:61–80.
Liu X, Lu B, Fu J, Zhu X, Song E, Song Y. Amorphous silica nanoparticles induce inflammation via activation of NLRP3 inflammasome and HMGB1/TLR4/MYD88/NF- κ b signaling pathway in HUVEC cells. J Hazard Mater 2021;404:124050.
Yang YL, Cheng X, Li WH, Liu M, Wang YH. Kaempferol attenuates LPS-induced striatum injury in mice involving anti-neuroinflammation, maintaining BBB integrity, and down-regulating the HMGB1/TLR4 pathway. Int J Mol Sci 2019;20:491.
Kong ZH, Chen X, Hua HP, Liang L, Liu LJ. The oral pretreatment of glycyrrhizin prevents surgery-induced cognitive impairment in aged mice by reducing neuroinflammation and Alzheimer’s-related pathology via HMGB1 inhibition. J Mol Neurosci 2017;63:385–395.
Paudel YN, Angelopoulou E, Piperi C, Othman I. Impact of HMGB1, RAGE, and TLR4 in Alzheimer’s Disease (AD): from risk factors to therapeutic targeting. Cells 2020;9:383.
Chou PS, Wu MN, Yang CC, Shen CT, Yang YH. Effect of advanced glycation end products on the progression of Alzheimer’s disease. J Alzheimer Dis 2019;72:191–197.
Yin QQ, Dong CF, Dong SQ, Dong XL, Hong Y, Hou XY, et al. AGEs induce cell death via oxidative and endoplasmic reticulum stresses in both human SH-SY5Y neuroblastoma cells and rat cortical neurons. Cell Mol Neurobiol 2012;32:1299–1309.
Author information
Authors and Affiliations
Contributions
Wang Y and Yang H conceived and designed the experiments. Wang Y, Wang Q, Luo D, Zhao P, Zhong SS, Dai B, and Wang JJ performed the experiments. Wang Y, Wang Q, Wan YT, and Liu ZB analyzed the data. Wang Y and Yang H contributed to the reagents and materials. Wan Y wrote the manuscript. All authors have read and approved the final version of the manuscript and consented to its publication.
Corresponding author
Ethics declarations
The authors declare that they have no competing interests.
Additional information
Supported by the National Natural Science Foundation of China (No. 82074552), Shaanxi Science and Technology Department Project (No. 2018JM7041), and Shaanxi Province TCM “Double Chain Integration” Young and Middle-Aged Scientific Research Innovation Team Construction Project (No. 2022-SLRH-LJ-012)
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Wang, Y., Wang, Q., Luo, D. et al. Electroacupuncture Improves Blood-Brain Barrier and Hippocampal Neuroinflammation in SAMP8 Mice by Inhibiting HMGB1/TLR4 and RAGE/NADPH Signaling Pathways. Chin. J. Integr. Med. 29, 448–458 (2023). https://doi.org/10.1007/s11655-023-3592-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-023-3592-5