Abstract
Objective
To assess the risk of aristolochic acid (AA)-associated cancer in patients with AA nephropathy (AAN).
Methods
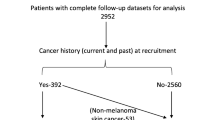
A retrospective study was conducted on patients diagnosed with AAN at Peking University First Hospital from January 1997 to December 2014. Long-term surveillance and follow-up data were analyzed to investigate the influence of different factors on the prevalence of cancer. The primary endpoint was the incidence of liver cancer, and the secondary endpoint was the incidence of urinary cancer during 1 year after taking AA-containing medication to 2014.
Results
A total of 337 patients diagnosed with AAN were included in this study. From the initiation of taking AA to the termination of follow-up, 39 patients were diagnosed with cancer. No cases of liver cancer were observed throughout the entire follow-up period, with urinary cancer being the predominant type (34/39, 87.17%). Logistic regression analysis showed that age, follow-up period, and diabetes were potential risk factors, however, the dosage of the drug was not significantly associated with urinary cancer.
Conclusions
No cases of liver cancer were observed at the end of follow-up. However, a high prevalence of urinary cancer was observed in AAN patients. Establishing a direct causality between AA and HCC is challenging.
Similar content being viewed by others
References
Vanherweghem JL, Depierreux M, Tielemans C, Abramowicz D, Dratwa M, Jadoul M, et al. Rapidly progressive interstitial renal fibrosis in young women: association with slimming regimen including Chinese herbs. Lancet 1993;341:387–391.
Boot A, Jiang N, Rozen SG. Toward clinical understanding of aristolochic acid upper-tract urothelial carcinoma. Theranostics 2020;10:5578–5580.
Lu H, Liang Y, Guan B, Shi Y, Gong Y, Li J, et al. Aristolochic acid mutational signature defines the low-risk subtype in upper tract urothelial carcinoma. Theranostics 2020;10:4323–4333.
Nault JC, Letouzé E. Mutational processes in hepatocellular carcinoma: the story of aristolochic acid. Semin Liver Dis 2019;39:334–340.
Bastek H, Zubel T, Stemmer K, Mangerich A, Beneke S, Dietrich DR. Comparison of aristolochic acid I derived DNA adduct levels in human renal toxicity models. Toxicology 2019;420:29–38.
Jadot I, Declèves AE, Nortier J, Caron N. An integrated view of aristolochic acid nephropathy: update of the literature. Int J Mol Sci 2017;18:297.
Schmeiser HH, Nortier JL, Singh R, Gamboa da Costa G, Sennesael J, Cassuto-Viguier E, et al. Exceptionally long-term persistence of DNA adducts formed by carcinogenic aristolochic acid I in renal tissue from patients with aristolochic acid nephropathy. Int J Cancer 2014;135:502–507.
Anger EE, Yu F, Li J. Aristolochic acid-induced nephrotoxicity: molecular mechanisms and potential protective approaches. Int J Mol Sci 2020;21:1157.
Zhao H, Jiang N, Han Y, Yang M, Gao P, Xiong X, et al. Aristolochic acid induces renal fibrosis by arresting proximal tubular cells in G2/M phase mediated by HIF-1 α. FASEB J 2020; 34:12599–12614.
Pu XY, Shen JY, Deng ZP, Zhang ZA. Oral exposure to aristolochic acid I induces gastric histological lesions with non-specific renal injury in rat. Exp Toxicol Pathol 2016;68:315–320.
Wang L, Li C, Tian J, Liu J, Zhao Y, Yi Y, et al. Genome-wide transcriptional analysis of aristolochia manshuriensis induced gastric carcinoma. Pharm Biol 2020;58:98–106.
Ng AWT, Poon SL, Huang MN, Lim JQ, Boot A, Yu W, et al. Aristolochic acids and their derivatives are widely implicated in liver cancers in Taiwan and throughout Asia. Sci Transl Med 2017;9:eaan6446.
Chen CJ, Yang YH, Lin MH, Lee CP, Tsan YT, Lai MN, et al. Herbal medicine containing aristolochic acid and the risk of hepatocellular carcinoma in patients with hepatitis B virus infection. Int J Cancer 2018;143:1578–1587.
Chen CJ, Yang YH, Lin MH, Lee CP, Tsan YT, Lai MN, et al. Herbal medicine containing aristolochic acid and the risk of primary liver cancer in patients with hepatitis C virus infection. Cancer Epidemiol Biomarkers Prev 2019;28:1876–1883.
Lu ZN, Luo Q, Zhao LN, Shi Y, Wang N, Wang L, et al. The mutational features of aristolochic acid-induced mouse and human liver cancers. Hepatology 2020;71:929–942.
Yang L, Su T, Li XM, Wang X, Cai SQ, Meng LQ, et al. Aristolochic acid nephropathy: variation in presentation and prognosis. Nephrol Dial Transplant 2012;27:292–298.
Ministry of Health of the People’s Republic of China. Updated standards for the diagnosis and treatment of primary liver cancer. Chin J Hepatol (Chin) 2020;33:112–128.
Na YQ, Sun G, eds. Chinese diagnosis and treatment of urological diseases guide. Beijing: People’s Medical Publishing House; 2009:3–115.
Ban TH, Min JW, Seo C, Kim DR, Lee YH, Chung BH, et al. Update of aristolochic acid nephropathy in Korea. Kor J Intern Med 2018;33:961–969.
Shan H, Tian W, Hong Y, Xu B, Wang C, Yu B, et al. Clinicopathologic characteristics and prognosis of upper tract urothelial carcinoma complicated with aristolochic acid nephropathy after radical nephroureterectomy. BMC Complement Med Ther 2020;20:166.
Zhang HM, Zhao XH, Sun ZH, Li GC, Liu GC, Sun LR, et al. Recognition of the toxicity of aristolochic acid. J Clin Pharm Ther 2019;44:157–162.
Hoang ML, Chen CH, Chen PC, Roberts NJ, Dickman KG, Yun BH, et al. Aristolochic acid in the etiology of renal cell carcinoma. Cancer Epidemiol Biomarkers Prev 2016;25:1600–1608.
Hu X, Shen J, Pu X, Zheng N, Deng Z, Zhang Z, et al. Urinary time- or dose-dependent metabolic biomarkers of aristolochic acid-induced nephrotoxicity in rats. Toxicol Sci 2017;156:123–132.
Fang ZE, Guo Y, Wang Z, He T, Wang J, Bai Z, et al. Asari Radix et Rhizoma consumption lacks relevance for hepatocellular carcinoma in patients: a retrospective cohort study. Chin Herb Med 2022;14:470–475.
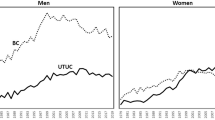
Xiong G, Yao L, Hong P, Yang L, Ci W, Liu L, et al. Aristolochic acid containing herbs induce gender-related oncological differences in upper tract urothelial carcinoma patients. Cancer Manag Res 2018;10:6627–6639.
Sun M, Zhang J, Zheng C, Liu Y, Lin F, Xu F, et al. Analysis of potential risk factors for cancer incidence in patients with aristolochic acid nephropathy from Wenzhou, China. Renal Failure 2015;37:209–213.
Bara TJr, Gurzu S, Sugimura H, Bara T, Beleaua MA, Jung I. A systematic review of the possible carcinogenic role of the aristolochic acid. Rom J Morphol Embryol 2017;58:41–44.
Acknowledgments
We would like to gratefully thank all patients for their trust and providing their respective data.
Author information
Authors and Affiliations
Contributions
Tao S and Fang ZE contributed equally to this work. Bai ZF, Yang L and Xiao XH contributed to the research conception and design. Su T, Fang ZE, and Guo YM participated in data interpretation and manuscript review and writing. Wang CY, Wang JB, and Ji D were responsible for data collection and analysis. All authors contributed to the scientific discussion of the data and of the manuscript.
Corresponding author
Ethics declarations
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Supported by National Key Technology R&D Program (No. 2018ZX09101002-001-002), Innovation Team and Talents Cultivation Program of National Administration of Traditional Chinese Medicine (No. ZYYCXTD-C-202005), the Science and Technology Project Affiliated to the Education Department of Chongqing Municipality (No. KJQN202215119)
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Su, T., Fang, Ze., Guo, Ym. et al. No Incidence of Liver Cancer Was Observed in A Retrospective Study of Patients with Aristolochic Acid Nephropathy. Chin. J. Integr. Med. 30, 99–106 (2024). https://doi.org/10.1007/s11655-023-3560-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-023-3560-0