Abstract
Objective
To assess the effects of Shenfu Injection (参附注射液, SFI) on blood lactate, and secondarily its effect on the lactate clearance (LC) in patients with post cardiac arrest syndrome (PCAS).
Methods
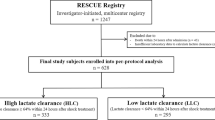
The present study is a post hoc study of a randomized, assessor-blinded, controlled trial. Patients experienced in-hospital cardiac arrest between 2012 and 2015 were included in the predefined post hoc analyses. Of 1,022 patients enrolled, a total of 978 patients were allocated to the control group (486 cases) and SFI (492 cases) group, receiving standardized post-resuscitation care bundle (PRCB) treatment or PRCB combined with SFI (100 mL/d), respectively. Patients’ serum lactate was measured simultaneously with artery blood gas, lactate clearance (LC) was calculated on days 1, 3, and 7 after admission and compared between groups. Lactate and LC were also compared between the survivors and non-survivors according to the 28-d mortality, as well as the survivors and non-survivors subgroups both in the SFI and control groups.
Results
In both groups, compared with pre-treatment levels, mean arterial pressure (MAP) and PaO2 were significantly improved on 1, 3, 7 d after treatment (P<0.05), while heart rate (HR) and blood glucose levels were significantly decreased on 1, 3 and 7 d after treatment (P<0.05). compared with control group, SFI treatment improved the values of MAP and PaO2 (P<0.05), and significantly decreased the levels of HR and the blood glucose level on 3 and 7 d after treatment (P<0.05). Compared with the control group, lactate levels decreased faster in the SFI group versus the control group on 3 and 7 d (P<0.05). From initiation of treatment and the following 3 and 7 d, SFI treatment greatly increased the LC compared with that in the control group (P<0.05). Compared with survivors, non-survivors had higher admission lactate levels (7.3 ±1.1 mmol/L vs. 5.5 ±2.3 mmol/L; P<0.01), higher lactate levels on days 1, 3 and 7 (P<0.05), and LC were decreased significantly on 3 and 7 d after treatment (P<0.05). Similar results were also found both in the SFI and control groups between survivors and non-survivors subgroups.
Conclusion
SFI in combination with PRCB treatment is effective at lowering lactate level and resulted in increasing LC in a targeted population of PCAS patients.
Similar content being viewed by others
Availability of Data and Materials
Please contact the authors for data requests.
References
Israelsson J, Bremer A, Herlitz J, Axellsson AB, Cronberg T, Djarv T, et al. Health status and psychological distress among in-hospital cardiac arrest survivors in relation to gender. Resuscitation 2017;114:27–33.
Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Bötiger BW, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation 2008;118:2452–2483.
Girotra S, Chan PS, Bradley SM. Post-resuscitation care following out-of-hospital and in-hospital cardiac arrest. Heart 2015;101:1943–1949.
Vermeulen RP, Hoekstra M, Nijsten MW, van der Horst IC, van Pelt J, Jessurun GA, et al. Clinical correlates of arterial lactate levels in patients with ST-segment elevation myocardial infarction at admission: a descriptive study. Crit Care 2010;14:R164.
Williams TA, Martin R, Celenza A, Alexandra B, Daniel F, Joel K, et al. Use of serum lactate levels to predict survival for patients with out-of-hospital cardiac arrest: a cohort study. Emerg Med Australas 2016;28:171–178.
Düring J, Dankiewicz J, Cronberg T, Hassager C, Hovdenes J, Kjaergaard J, et al. Lactate, lactate clearance and outcome after cardiac arrest: a post-hoc analysis of the TTM-Trial. Acta Anaesthesiol Scand 2018;62:1436–1442.
Morley PT. The promise of traditional Chinese medicine after cardiac arrest: an untapped resource? Crit Care Med 2017;45:1772–1773.
Yang H, Liu L, Gao W, Liu K, Qi LW, Li P. Direct and comprehensive analysis of ginsenosides and diterpene alkaloids in Shenfu injection by combinatory liquid chromatography-mass spectrometric techniques. J Pharm Biomed Anal 2014;92:13–21.
Mou ZJ, Lv ZT, Li Y, Wang M, Xu Q, Yu XZ. Clinical effect of Shenfu Injection in patients with septic shock: a meta-analysis and systematic review. Evid Based Complement Alternat Med 2015;2015:863149.
Zhang Q, Li C, Shao F, Zhao L, Wang M, Fang Y. Efficacy and safety of combination therapy of Shenfu Injection and postresuscitation bundle in patients with return of spontaneous sirculation after in-hospital cardiac arrest: a randomized, assessor-blinded, controlled trial. Crit Care Med 2017;45:1587–1595.
Koster RW, Baubin MA, Bossaert LL, Caballero AN, Cassan PA, Castrén MA, et al. European Resuscitation Council guidelines for resuscitation 2010 section 2. adult basic life support and use of automated external defibrillators. Resuscitation 2010;81:1277–1292.
Cummins RO, Chamberlain D, Hazinski MF, Nadkani V, Kloeck W, Kramer E, et al. American Heart Association. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein style.” Circulation 1997;95:2213–2239.
Akhter S, Warraich UA, Ghazal S, Rizvi N. Assessment and comparison of APACHE II (Acute Physiology and Chronic Health Evaluation), SOFA (Sequential Organ Failure Assessment) score and CURB 65 (confusion; urea; respiratory rate; blood pressure), for prediction of inpatient mortality in acute exacerbation of chronic obstructive pulmonary disease. J Pak Med Assoc 2019;69:211–215.
Pothiawala S. Post-resuscitation care. Singapore Med J 2017;58:404–407.
Walker AC, Johnson NJ. Critical care of the post-cardiac arrest patient. Cardiol Clin 2018;36:419–428.
Starodub R, Abella BS, Grossestreuer AV, Frances SS, Sarah MP, Marion L, et al. Association of serum lactate and survival outcomes in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation 2013;84:1078–1082.
Lokhandwala S, Andersen LW, Nair S, Patel P, Cocchi MN, Donnino MW. Absolute lactate value vs relative reduction as a predictor of mortality in severe sepsis and septic shock. J Crit Care 2017;37:179–184.
Hayashida K, Suzuki M, Yonemoto N, Hori S, Tanura T, Sakurai A, et al. Where effective lactate reduction over the first 6 hours of postcardiac arrest care was associated with survival and good neurologic outcome. Crit Care Med 2017;45:e559–e566.
Shapiro NI, Howell MD, Talmor D, Larry AN, Alan L, Richaro EW, et al. Serum lactate as a predictor of mortality in emergency department patients with infection. Ann Emerg Med 2005;45:524–528.
Guo ZJ, Li CS. Therapeutic effects of Shenfu Injection on post-cardiac arrest syndrome. Chin J Integr Med 2013;19:716–720.
Zhang Q, Li C. The roles of traditional Chinese medicine: Shenfu injection on the postresuscitation care bundle. Evid Based Complement Alternat Med 2013;2013:319092.
Zheng SD, Wu HJ, Yu SP, Ren JX, Duo WW, Ma ZC, et al. Shenfu Injection suppresses inflammation by targeting haptoglobin and pentraxin 3 in rats with chronic ischemic heart failure. Chin J Integr Med 2015;21:22–28.
Jin YY, Gao H, Zhang XY, Ai H, Zhu XL, Wang J. Shenfu Injection inhibits inflammation in patients with acute myocardial infarction complicated by cardiac shock. Chin J Integr Med 2017;23:170–175.
Huang P, Guo Y, Feng S, Zhao G, Li B, Liu Q. Efficacy and safety of Shenfu injection for septic shock: a systematic review and meta-analysis of randomized controlled trials. Am J Emerg Med 2019;37:2197–2204.
Li MQ, Pan CG, Wang XM, Mo X, Shi ZX, Xu JY, et al. Effect of the Shenfu Injection combined with early goal-directed therapy on organ functions and outcomes of septic shock patients. Cell Biochem Biophys 2015;72:807–812.
Li YH, Yu B, Duan ZZ, Olunga MA, Jia H, Zhou K, et al. The coronary dilation effect of shenfu injection was mediated through NO. PLoS One 2014;9:e92415.
Wang T, Yu XF, Qu SC, Xu HL, Sui DY. Ginsenoside Rb3 inhibits angiotensin II-induced vascular smooth muscle cells proliferation. Basic Clin Pharmacol Toxicol 2010;107:685–689.
Guo Z, Wu C, Li C. Shen-Fu injection alleviates post-resuscitation myocardial dysfunction by up-regulating expression of sarcoplasmic reticulum Ca2+-ATPase. Chin J Integr Med 2016;22:503–509.
Ji XF, Yang L, Zhang MY, Li CS, Wang S, Cong LH, et al. Shen-fu injection attenuates postresuscitation myocardial dysfunction in a porcine model of cardiac arrest. Shock 2011;35:530–536.
Wei H, Wu H, Yu W, Yan X, Zhang X. Shenfu decoction as adjuvant therapy for improving quality of life and hepatic dysfunction in patients with symptomatic chronic heart failure. J Ethnopharmacol 2015;169:347–355.
Author information
Authors and Affiliations
Contributions
Conception and design: Zhang Q; collection and assembly of data: Zhang Q and He Y; data analysis and interpretation: Zhang Q, He Y and Wang GX; literature review: He Y and Wang YX; manuscript writing: all authors; critical review: Zhang Q; final approval of manuscript: all authors.
Corresponding author
Additional information
Conflict of Interest
The funders had no role in the study design, data collection and analysis, decision to publish or preparation of the manuscript. No extramural funding was used to support this work. The authors are solely responsible for the design and conduct of this study; all study analyses, the drafting and editing of the manuscript, and its final contents.
Supported by the Beijing Municipal Administration of Hospitals’ Youth Programme (No. QML20170301)
Rights and permissions
About this article
Cite this article
He, Y., Wang, Gx., Li, C. et al. Effect of Shenfu Injection (参附注射液) on Lactate and Lactate Clearance in Patients with Post-cardiac Arrest Syndrome: A Post Hoc Analysis of a Multicenter Randomized Controlled Trial. Chin. J. Integr. Med. 28, 894–899 (2022). https://doi.org/10.1007/s11655-021-3455-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-021-3455-x