Abstract
Objective
To investigate the ameliorate effect and underlying mechanism of Xueshuantong for Injection (Lyophilized, 注射用血栓通, XST) in streptozocin (STZ)-induced diabetic retinopathy (DR) rats.
Methods
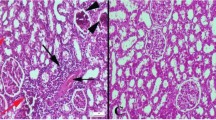
Diabetes mellitus (DM) model was induced by intraperitoneal (i.p.) injection of STZ (60 mg/kg) in Sprague-Dawley rats. Diabetic rats were randomized into 3 groups (n=10) according to a random number table, including DM, XST50 and XST100 groups. XST treatment groups were daily i.p. injected with 50 or 100 mg/kg XST for 60 days, respectively. The control and DM groups were given i.p. injection with saline. Blood glucose level and body weight were recorded every week. Histological changes in the retina tissues were observed with hematoxylin-eosin staining. Apoptosis and inflammation related factors, including cleaved caspase-3, glial fifibrillary acidic protein (GFAP), tumor necrosis factor-α (TNF-α) and intercellular cell adhesion molecule-1 (ICAM-1) were detected by Western blot or real-time polymerase chain reaction. Then, the levels of advanced glycation end product (AGE) and its receptor (RAGE) were investigated. Tight junctions proteins (Zonula occludens-1 (ZO-1), Occludin and Claudin-5) of blood-retinal barrier were detected by Western blot. The levels of retinal fifibrosis, transforming growth factor-β1 (TGF-β1)-Smad2/3 signaling pathway were evaluated at last.
Results
There was no signifificant difference in the body weight and blood glucose level between XST and DM groups (P>0.05). Compared with the DM group, XST treatment signifificantly increased the retinal thickness of rats (P<0.05 or P<0.01), and suppressed cleaved caspase-3 expression (P<0.01). XST increased the protein expressions of ZO-1, Occludin and Claudin-5 and decreased the mRNA expressions of matrix metalloproteinase 2 (MMP-2) and MMP-9 (P<0.05 or P<0.01). Moreover, XST signifificantly reduced the productions of AGE and RAGE proteins in the retina of rats (P<0.05 or P<0.01), suppressed the over-expression of TNF-α, and decreased the elevated level of ICAM-1 in retina of rats (P<0.05 or P<0.01). XST signifificantly reduced the levels of α-smooth muscle actin (α-SMA), connective tissue growth factor (CTGF), TGF-β1 and phosphorylation of Smad2/3 protein in rats (P<0.05 or P<0.01).
Conclusions
XST had protective effects on DR with possible mechanisms of inhibiting the inflammation and apoptosis, up-regulating the expression of tight junction proteins, suppressing the productions of AGE and RAGE proteins, and blocking the TGF-β/Smad2/3 signaling pathway. XST treatment might play a role for the future therapeutic strategy against DR.
Similar content being viewed by others
References
Perleberg C, Kind A, Schnieke A. Genetically engineered pigs as models for human disease. Dis Model Mech 2018;11:030783.
Park SW, Yun JH, Kim JH, Kim KW, Cho CH, Kim JH. Angiopoietin 2 induces pericyte apoptosis via α3β1 integrin signaling in diabetic retinopathy. Diabetes 2014;63:3057–3068.
Bai L, Gao J, Wei F, Zhao J, Wang D, Wei J. Therapeutic potential of ginsenosides as an adjuvant treatment for diabetes. Front Pharmacol 2018;9:423.
Lou J, Wang Y, Zhang Z, Qiu W. Activation of MMPs in macrophages by Mycobacterium tuberculosis via the miR-223-BMAL1 signaling pathway. J Cell Biochem 2017;118:4804–4812.
Giebel SJ, Menicucci G, McGuire PG, Das A. Matrix metalloproteinases in early diabetic retinopathy and their role in alteration of the blood-retinal barrier. Lab Invest 2005;85:597–607.
Prasad K, Dhar I, Zhou Q, Elmoselhi H, Shoker M, Shoker A. AGEs/sRAGE, a novel risk factor in the pathogenesis of endstage renal disease. Mol Cell Biochem 2016;423:105–114.
Ding H, Bai F, Cao H, Xu J, Fang L, Wu J, et al. PDE/cAMP/Epac/C/EBP-beta signaling cascade regulates mitochondria biogenesis of tubular epithelial cells in renal fibrosis. Antioxid Redox Signal 2018;29:637–652.
Gao L, Zhao H, Liu Q, Song J, Xu C, Liu P, et al. Improvement of hematoma absorption and neurological function in patients with acute intracerebral hemorrhage treated with Xueshuantong. J Neurol Sci 2012;323:236–240.
Yin Y, Chen F, Wang W, Wang H, Zhang X. Resolvin D1 inhibits inflammatory response in STZ-induced diabetic retinopathy rats: possible involvement of NLRP3 inflammasome and NF-κB signaling pathway. Mol Vis 2017;23:242–250.
Wang X, Wang S, Wang J, Guo H, Dong Z, Chai L, et al. Neuroprotective effect of Xueshuantong for Injection (Lyophilized) in transient and permanent rat cerebral ischemia model. Evid Based Complement Alternat Med 2015;2015:134685.
Koleva-Georgieva DN, Sivkova NP, Terzieva D. Serum inflammatory cytokines IL-1beta, IL-6, TNF-alpha and VEGF have influence on the development of diabetic retinopathy. Folia Med (Plovdiv) 2011;53:44–50.
Das UN. Is lipoxins A(4) a better alternative to anti-VEGF and anti-TNF-alpha antibody to prevent and treat agerelated macular degeneration, diabetic macular edema and retinopathy? Med Sci Monit 2012;18:LE1–2.
Adamiec-Mroczek J, Zajac-Pytrus H, Misiuk-Hojlo M. Caspasedependent apoptosis of retinal ganglion cells during the development of diabetic retinopathy. Adv Clin Exp Med 2015;24:531–535.
Zhang Q, Steinle JJ. IGFBP-3 inhibits TNF-alpha production and TNFR-2 signaling to protect against retinal endothelial cell apoptosis. Microvasc Res 2014;95:76–81.
Bucolo C, Marrazzo G, Platania CB, Drago F, Leggio GM, Salomone S. Fortified extract of red berry, Ginkgo biloba, and white willow bark in experimental early diabetic retinopathy. J Diabetes Res 2013;2013:432695.
Ghadiri Soufi F, Arbabi-Aval E, Rezaei Kanavi M, Ahmadieh H. Anti-inflammatory properties of resveratrol in the retinas of type 2 diabetic rats. Clin Exp Pharmacol Physiol 2015;42:63–68.
Hossain A, Tauhid L, Davenport I, Huckaba T, Graves R, Mandal T, et al. LRP-1 pathway targeted inhibition of vascular abnormalities in the retina of diabetic mice. Curr Eye Res 2017;42:640–647.
Liang LN, Bai YY, Tang YZ, Chen C, Li XL, Ma QY, et al. Contribution of Borneolum syntheticum to the intervention effect of Liuwei Dihuang Pill on experimental retinal degeneration. Chin J Integr Med 2018;24:442–447.
Shi X, Liao S, Mi H, Guo C, Qi D, Li F, et al. Hesperidin prevents retinal and plasma abnormalities in streptozotocininduced diabetic rats. Molecules 2012;17:12868–12881.
Joussen AM, Smyth N, Niessen C. Pathophysiology of diabetic macular edema. Dev Ophthalmol 2007;39:1–12.
Kim J, Kim CS, Lee YM, Jo K, Shin SD, Kim JS. Methylglyoxal induces hyperpermeability of the blood-retinal barrier via the loss of tight junction proteins and the activation of matrix metalloproteinases. Graefes Arch Clin Exp Ophthalmol 2012;250:691–697.
Das A, Stroud S, Mehta A, Rangasamy S. New treatments for diabetic retinopathy. Diabetes Obes Metab 2015;17:219–230.
Aktas HS, Ucak S, Demirbas MB, Sarikaya Z, Olcum GG, Pinar E. The relation of protein C and protein S levels with cardiovascular risk in patients with diabetic neuropathy. Diabetes Metab Syndr 2016;10:234–237.
Zhao J, Randive R, Stewart JA. Molecular mechanisms of AGE/ RAGE-mediated fibrosis in the diabetic heart. World J Diabetes 2014;5:860–867.
Lan HY, Chung AC. Transforming growth factor-beta and Smads. Contrib Nephrol 2011;170:75–82.
Wang L, Chi YF, Yuan ZT, Zhou WC, Yin PH, Zhang XM, et al. Astragaloside IV inhibits renal tubulointerstitial fibrosis by blocking TGF-beta/Smad signaling pathway in vivo and in vitro. Exp Biol Med (Maywood) 2014;239:1310–1324.
Zhu J, Nguyen D, Ouyang H, Zhang XH, Chen XM, Zhang K. Inhibition of RhoA/Rho-kinase pathway suppresses the expression of extracellular matrix induced by CTGF or TGF-beta in ARPE-19. Int J Ophthalmol 2013;6:8–14.
Gerhardinger C, Dagher Z, Sebastiani P, Park YS, Lorenzi M. The transforming growth factor-beta pathway is a common target of drugs that prevent experimental diabetic retinopathy. Diabetes 2009;58:1659–1667.
Fan JS, Liu DN, Huang G, Xu ZZ, Jia Y, Zhang HG, et al. Panax notoginseng saponins attenuate atherosclerosis via reciprocal regulation of lipid metabolism and inflammation by inducing liver X receptor alpha expression. J Ethnopharmacol 2012;142:732–738.
Ning N, Dang X, Bai C, Zhang C, Wang K. Panax notoginsenoside produces neuroprotective effects in rat model of acute spinal cord ischemia-reperfusion injury. J Ethnopharmacol 2012;139:504–512.
Dai JP, Chen XX, Zhu DX, Wan QY, Chen C, Wang GF, et al. Panax notoginseng saponins inhibit areca nut extract-induced oral submucous fibrosis in vitro. J Oral Pathol Med 2014;43:464–470.
Hui J, Gao J, Wang Y, Zhang J, Han Y, Wei L, et al. Panax notoginseng saponins ameliorates experimental hepatic fibrosis and hepatic stellate cell proliferation by inhibiting the Jak2/Stat3 pathways. J Tradit Chin Med 2016;36:217–224.
Author information
Authors and Affiliations
Contributions
Li RL analyzed the data and drafted the manuscript; Wang JX contributed in performing the experiments. Wang SX conceived and designed the experiments and revised the manuscript. Wang H and Chen L performed the HE staining test and revised the manuscript; Chai LJ and Guo H participated in the test of tight junction proteins; Hu LM supervised and coordinated all studies. All authors read the manuscript and approved the submission.
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Additional information
Supported by the National Natural Science Foundation of China (No. 81573644), Major New Drugs Innovation and Development (No. 2012ZX09101201-004), Guangxi Provincial Department of Science and Technology (No. 14125008-2-5), and Tianjin 131 Innovative Team Project and Training Program Foundation for Innovative Research Team of Higher Education in Tianjin (No. TD13-5050)
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Li, Rl., Wang, Jx., Chai, Lj. et al. Xueshuantong for Injection (Lyophilized, 注射用血栓通) Alleviates Streptozotocin-Induced Diabetic Retinopathy in Rats. Chin. J. Integr. Med. 26, 825–832 (2020). https://doi.org/10.1007/s11655-020-3088-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-020-3088-5