Abstract
Objective
To examine the effect of moxibustion on the wound healing process and its mechanism using a rat wound model.
Methods
Sixty male Sprague-Dawley rats were randomly divided into a sham-treated group (n=30, wound surgery only) and a moxibustion group (n=30, wound treated with moxibustion). Circular full-thickness skin wounds were produced in rats. Moxibustion was applied to the edge of wound and was continued on alternating days till 14 days after surgery, followed by measurement of wound size. Expression of collagens, prolyl-4-hydroxylase (P4H) and transforming growth factor-β (TGF-β) were evaluated by histochemical study and real-time polymerase chain reaction.
Results
The size of the wound lesion was significantly reduced in rats treated with moxibustion as compared to that in sham-treated rats at 4–10 days after wounding (P<0.01). Moxibustion stimulated mRNA expression of collagens at 4 days (P<0.01), but not at 7 days, accompanied by enhanced proliferation of P4H-positive fibroblasts. Of importance, expression of TGF-β in tissue from the wound lesion treated with moxibustion was significantly increased as compared to that in sham-treated rats at 4 days (P<0.01 or P<0.05), but not at 7 days.
Conclusions
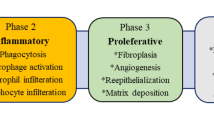
The treatment with moxibustion promoted the wound healing process in the early phase through proliferation of fibroblasts and rapid formation of granulation, possibly mediated by induction of TGF-β which is a key molecule in the physiological process of wound healing. Moxibustion can be expected to be effective as complementary treatment for intractable ulcers.
Similar content being viewed by others
References
Ma Y, Dong M, Zhou K, Mita C, Liu J, Wayne PM. Publication trends in acupuncture research: a 20-year bibliometric analysis based on PubMed. PLoS One 2016;11:e0168123.
Shu Q, Wang H, Litscher D, Wu S, Chen L, Gaischek I, et al. Acupuncture and moxibustion have different effects on fatigue by regulating the autonomic nervous system: a pilot controlled clinical trial. Sci Rep 2016;25:37846.
Yao M, Sun YL, Dun RL, Lan TY, Li JL, Lee HJ, et al. Is manipulative therapy clinically necessary for relief of neck pain? A systematic review and meta-analysis. Chin J Integr Med 2017;23:543–554.
Chen HY, Liu NY. Analgesic effect of sinew acupuncture for patients with soft-tissue injuries: a pilot trial. Chin J Integr Med 2019;25:613–616.
Kim SY, Chae Y, Lee SM, Lee H, Park HJ. The effectiveness of moxibustion: an overview during 10 years. Evid Based Complement Alternat Med 2011;2011:306515.
Gao XY, Chong CY, Zhang SP, Cheng KW, Zhu B. Temperature and safety profiles of needle-warming techniques in acupuncture and moxibustion. Evid Based Complement Alternat Med 2012;2012:168393.
Bao C, Liu P, Liu H, Jin X, Calhoun VD, Wu L, et al. Different brain responses to electro-acupuncture and moxibustion treatment in patients with Crohn’s disease. Sci Rep 2016;18:36636.
Yang X, Xiong X, Yang G, Wang J. Effectiveness of stimulation of acupoint KI 1 by Artemisia vulgaris (Moxa) for the treatment of essential hypertension: a systematic review of randomized controlled trials. Evid Based Complement Alternat Med 2014;2014:187484.
Xiong X, Liu W, Yang X, Feng B, Wang J. Moxibustion for essential hypertension. Complement Ther Med 2014;22:187–195.
Kim HG, Yoo SR, Park HJ, Son CG. Indirect moxibustion (CV4 and CV8) ameliorates chronic fatigue: a randomized, double-blind, controlled study. J Altern Complement Med 2013;19:134–140.
Kim TH, Choi TY, Shin BC, Lee MS. Moxibustion for managing type 2 diabetes mellitus: a systematic review. Chin J Integr Med 2011;17:575–579.
Yang M, Chen X, Bo L, Lao L, Chen J, Yu S, et al. Moxibustion for pain relief in patients with primary dysmenorrhea: a randomized controlled trial. PLoS One 2017;12:e0170952.
Chen R, Chen M, Xiong J, Chi Z, Zhou M, Su T, et al. Is there difference between the effects of two-dose stimulation for knee osteoarthritis in the treatment of heat-sensitive moxibustion? Evid Based Complement Alternat Med 2012;2012:696498.
Yamashita H, Ichiman Y, Tanno Y. Changes in peripheral lymphocyte subpopulations after direct moxibustion. Am J Chin Med 2001;29:227–235.
Reinke JM, Sorg H. Wound repair and regeneration. Eur Surg Res 2012;49:35–43.
Sun YH, Sun YH, Sun LH, Liang YL, Zhao ZS, Zhang HZ, et al. Effect of mild-warm moxibustion on microcirculation in the raw surface tissue of chronic refractory wound in skin ulcer rats. Acupunct Res (Chin) 2011;36:321–326.
Guo XT, Dong QJ, Cao YQ. Effects of mild moxibustion on angiogenesis and microcirculation in wound repair after operation of anal fistula in rats. J Chin Integr Med (Chin) 2009;7:1154–1158.
Sun Q, Sun ZR, Zhang QH, Wang D, Yue JH. Effect of moxibustion on vascular endothelial cell and expression of vascular endothelial growth factor in rats with cutaneous wound. Chin Acupunct Moxibust (Chin) 2014;34:679–684.
Sun LH, Liang YL, Sun YH, Sun YH, Zhang HZ, Li XF, et al. Effect of mild moxibustion on macrophage number and collagen expression of raw surface tissue in chronic refractory skin ulcer rats. Acupunct Res (Chin) 2012;37:259–265.
Kang LR, Ba HY. Moxibustion on the selected points according to meridians for pressure ulcers of 15 cases. J Clin Acupunct Moxibust 2004;20:22.
Zhang QH, Yue JH, Li CR, Sun ZR. Moxibustion for the treatment of pressure ulcers: study protocol for a pilot, multicentre, randomised controlled trial. BMJ Open 2014;4:e006423.
Wang PH, Huang BS, Horng HC, Yeh CC, Chen YJ. Wound healing. J Chin Med Assoc 2018;81:94–101.
Mori HM, Kawanami H, Kawahata H, Aoki M. Wound healing potential of lavender oil by acceleration of granulation and wound contraction through induction of TGF-β in a rat model. BMC Complement Altern Med 2016;26:144.
Heinemeier KM, Olesen JL, Haddad F, Schjerling P, Baldwin KM, Kjaer M. Effect of unloading followed by reloading on expression of collagen and related growth factors in rat tendon and muscle. J Appl Physiol 2009;106:178–186.
Monaco JL, Lawrence WT. Acute wound healing: an overview. Clin Plastic Surg 2003;30:1–12.
Clark RAF, ed. Overview and general consideration of wound repair. The molecular and cell biology of wound repair. 2nd ed. New York: Plenum Press;1996:3–50.
Sinno H, Prakash S. Complements and the wound healing cascade: an updated review. Plast Surg Int 2013:146764.
Rousselle P, Montmasson M, Garnier C. Extracellular matrix contribution to skin wound re-epithelialization. Matrix Biol 2019;75–76:12–26.
Martin P, Nunan R. Cellular and molecular mechanisms of repair in acute and chronic wound healing. Br J Dermatol 2015;173:370–378.
Haylor J, Schroeder J, Wagner B, Nutter F, Jestin G, Idée JM, et al. Skin gadolinium following use of MR contrast agents in a rat model of nephrogenic systemic fibrosis. Radiology 2012;263:107–116.
Anantharajan J, Koski MK, Kursula P, Hieta R, Bergmann U, Myllyharju J, et al. The structural motifs for substrate binding and dimerization of the a subunit of collagen prolyl 4-hydroxylase. Structure 2013;21:2107–2118.
Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev 2003;83:835–870.
Barrientos S, Stojadinovic O, Golinko MS, Brem H, Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen 2008;16:585–601.
Finnson KW, McLean S, Di Guglielmo GM, Philip A. Dynamics of transforming growth factor beta signaling in wound healing and scarring. Adv Wound Care (New Rochelle) 2013;2:195–214.
Alves CC, Torrinhas RS, Giorgi R, Brentani MM, Logullo AF, Waitzberg DL. TGF-β 1 expression in wound healing is acutely affected by experimental malnutrition and early enteral feeding. Int Wound J 2014;11:533–539.
Bielefeld KA, Amini-Nik S, Alman BA. Cutaneous wound healing: recruiting developmental pathways for regeneration. Cell Mol Life Sci 2013;70:2059–2081.
Ehanire T, Ren L, Bond J, Medina M, Li G, Bashirov L, et al. Angiotensin II stimulates canonical TGF-β signaling pathway through angiotensin type 1 receptor to induce granulation tissue contraction. J Mol Med (Berl) 2015;93:289–302.
Hu F, Yan Y, Wang CW, Liu Y, Wang JJ, Zhou F, et al. Effect and mechanism of ganoderma lucidum polysaccharides on human fibroblasts and skin wound healing in mice. Chin J Integr Med 2019;25:203–209.
Xue M, Jackson CJ. Extracellular matrix reorganization during wound healing and its impact on abnormal scarring. Adv Wound Care (New Rochelle) 2015;4:119–136.
Leask A. The contribution of peroxisome proliferator-activated receptor gamma to cutaneous wound healing. Adv Wound Care (New Rochelle) 2013;2:69–73.
Li G, Li YY, Sun JE, Lin WH, Zhou RX. ILK-PI3K/AKT pathway participates in cutaneous wound contraction by regulating fibroblast migration and differentiation to myofibroblast. Lab Invest 2016;96:741–751.
Author information
Authors and Affiliations
Contributions
Kawanami H conceived and designed the experiments, carried out the laboratory experiments, analyzed and interpreted the data, and prepared the manuscript. Kawahata H and Mori HM analyzed and interpreted the data, and prepared the manuscript. Aoki M conceived and designed the experiments, analyzed and interpreted the data, and revised the article critically for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Additional information
Conflict of Interest
The authors declare that they have no competing interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Kawanami, H., Kawahata, H., Mori, HM. et al. Moxibustion Promotes Formation of Granulation in Wound Healing Process through Induction of Transforming Growth Factor-β in Rats. Chin. J. Integr. Med. 26, 26–32 (2020). https://doi.org/10.1007/s11655-019-3083-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11655-019-3083-x