Abstract
Background
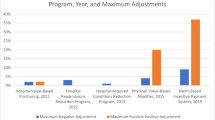
Medicare’s voluntary bundled payment programs have demonstrated generally favorable results. However, it remains unknown whether uneven hospital participation in these programs in communities with greater shares of minorities and patients of low socioeconomic status results in disparate access to practice redesign innovations.
Objective
Examine whether communities with higher proportions of marginalized individuals were less likely to be served by a hospital participating in Bundled Payments for Care Improvement Advanced (BPCI-Advanced).
Design
Cross-sectional study using ordinary least squares regression controlling for patient and community factors.
Participants
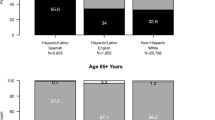
Medicare fee-for-service patients enrolled from 2015–2017 (pre-BPCI-Advanced) and residing in 2,058 local communities nationwide defined by Hospital Service Areas (HSAs). Each community’s share of marginalized patients was calculated separately for each of the share of beneficiaries of Black race, Hispanic ethnicity, or dual eligibility for Medicare and Medicaid.
Main Measures
Dichotomous variable indicating whether a given community had at least one hospital that ever participated in BPCI-Advanced from 2018–2022.
Key Results
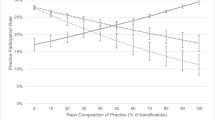
Communities with higher shares of dual-eligible individuals were less likely to be served by a hospital participating in BPCI-Advanced than communities with the lowest quartile of dual-eligible individuals (Q4: -15.1 percentage points [pp] lower than Q1, 95% CI: -21.0 to -9.1, p < 0.001). There was no consistent significant relationship between community proportion of Black beneficiaries and likelihood of having a hospital participating in BPCI-Advanced. Communities with higher shares of Hispanic beneficiaries were more likely to have a hospital participating in BPCI-Advanced than those in the lowest quartile (Q4: 19.2 pp higher than Q1, 95% CI: 13.4 to 24.9, p < 0.001).
Conclusions
Communities with greater shares of dual-eligible beneficiaries, but not racial or ethnic minorities, were less likely to be served by a hospital participating in BPCI-Advanced Policymakers should consider approaches to incentivize more socioeconomically uniform participation in voluntary bundled payments.



Similar content being viewed by others
References
What Are Bundled Payments? NEJM Catalyst. 2018. https://doi.org/10.1056/CAT.18.0247
Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Year 1 of the Bundled Payments for Care Improvement–Advanced Model. N Engl J Med. 2021;385(7):618-627.https://doi.org/10.1056/NEJMsa2033678.
Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Evaluation of Medicare’s Bundled Payments Initiative for Medical Conditions. N Engl J Med. 2018;379(3):260-269.https://doi.org/10.1056/NEJMsa1801569.
CMS Bundled Payments for Care Improvement Advanced Model: Third Evaluation Report. Lewin Group 2022:1–84. Accessed January 14, 2023. https://innovation.cms.gov/data-and-reports/2022/bpci-adv-ar3.
Liao JM, Ibrahim SA, Huang Q, et al. The Proportion of Marginalized Individuals in US Communities and Hospital Participation in Bundled Payments. Popul Health Manag. 2022;25(4):501–508. (In eng). https://doi.org/10.1089/pop.2021.0334.
Liao JM, Huang Q, Ibrahim SA, et al. Between-Community Low-Income Status and Inclusion in Mandatory Bundled Payments in Medicare’s Comprehensive Care for Joint Replacement Model. JAMA Network Open 2021;4(3):e211016-e211016. https://doi.org/10.1001/jamanetworkopen.2021.1016.
Innovation Center Strategy Refresh. Center for Medicare and Medicaid Innovation (CMMI). 2021. Accessed September 5, 2023. https://innovation.cms.gov/strategic-direction-whitepaper.
BPCI Advanced. Centers for Medicare & Medicaid Services. Accessed September 5, 2023. https://innovation.cms.gov/innovation-models/bpci-advanced.
Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Characteristics of Hospitals That Did and Did Not Join the Bundled Payments for Care Improvement–Advanced Program. JAMA 2019;322(4):362-364. https://doi.org/10.1001/jama.2019.7992.
CMS Bundled Payments for Care Improvement Advanced Model: Fourth Evaluation Report. Lewin Group 2023:1–117. Accessed December 27, 2023. https://www.cms.gov/priorities/innovation/data-and-reports/2023/bpci-adv-ar4.
Elm Ev, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335(7624):806–808. https://doi.org/10.1136/bmj.39335.541782.AD.
Bureau C. American Community Survey. https://www.census.gov/programs-surveys/acs/data.html.
The Dartmouth Atlas of Health Care. The Center for the Evaluative Clinical Sciences, Dartmouth Medical School; 1996. Accessed January 6, 2023. https://www.dartmouthatlas.org/.
Chamberlain G. Analysis of Covariance with Qualitative Data. Rev Econ Stud. 1980;47(1):225–238. https://EconPapers.repec.org/RePEc:oup:restud:v:47:y:1980:i:1:p:225-238.
Bundled Payments for Care Improvement Advanced: General Frequently Asked Questions (FAQs). Centers for Medicare & Medicaid Services (CMS). Accessed September 5, 2023. https://www.cms.gov/priorities/innovation/files/x/bpci-advanced-faqs.pdf.
Roberts ET, Song Z, Ding L, McWilliams JM. Changes in patient experiences and assessment of gaming among large clinician practices in precursors of the Merit-Based Incentive Payment System. JAMA Health Forum 2021;2(10):. (In eng). https://doi.org/10.1001/jamahealthforum.2021.3105.
Johnston KJ, Hockenberry JM, Wadhera RK, Joynt Maddox KE. Clinicians With High Socially At-Risk Caseloads Received Reduced Merit-Based Incentive Payment System Scores. Health Aff. 2020;39(9):1504-1512. https://doi.org/10.1377/hlthaff.2020.00350.
Laura C, Yasaitis WP, Polsky D, Werner RM. Physicians’ Participation In ACOs Is Lower In Places With Vulnerable Populations Than In More Affluent Communities. Health Affairs 2016;35(8):1382–1390. https://doi.org/10.1377/hlthaff.2015.1635.
Hammond G, Orav EJ, Zheng J, Epstein AM, Joynt Maddox KE. Changes in Racial Equity Associated With Participation in the Bundled Payments for Care Improvement Advanced Program. JAMA Network Open 2022;5(12):e2244959-e2244959. https://doi.org/10.1001/jamanetworkopen.2022.44959.
Navathe AS, Liao JM, Polsky D, et al. Comparison Of Hospitals Participating In Medicare’s Voluntary And Mandatory Orthopedic Bundle Programs. Health Aff. 2018;37(6):854-863. https://doi.org/10.1377/hlthaff.2017.1358.
Gondi S, Joynt Maddox K, Wadhera RK. “REACHing” for Equity — Moving from Regressive toward Progressive Value-Based Payment. N Engl J Med. 2022;387(2):97-99. https://doi.org/10.1056/NEJMp2204749.
Markovitz AA, Hollingsworth JM, Ayanian JZ, et al. Risk Adjustment In Medicare ACO Program Deters Coding Increases But May Lead ACOs To Drop High-Risk Beneficiaries. Health Aff (Millwood). 2019;38(2):253–261. (In eng). https://doi.org/10.1377/hlthaff.2018.05407.
Navathe AS, Schmidt H. Why a Hospital Might Shun a Black Patient. The New York Times 2020:Section A:27. (Opinion). https://www.nytimes.com/2020/10/06/opinion/medical-racism-payment-models.html
Kilaru AS, Wiebe DJ, Karp DN, Love J, Kallan MJ, Carr BG. Do hospital service areas and hospital referral regions define discrete health care populations? Med Care 2015;53(6):510–6. (In eng). https://doi.org/10.1097/mlr.0000000000000356.
Funding
This work was funded by the National Institute on Minority Health and Health Disparities (R01-MD013859 and R01-MD015055) and Agency for Health Research and Quality (R01HS027595). Dr. Kilaru received support from the Agency for Healthcare Research and Quality (5K12HS026372-04). Sponsors did not have any role in the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest:
Dr. Navathe reports grants from Hawaii Medical Service Association, grants from Commonwealth Fund, grants from Robert Wood Johnson Foundation, grants from Donaghue Foundation, grants from the Veterans Affairs Administration*, grants from Arnold Ventures, grants from United Healthcare, grants from Blue Cross Blue Shield of NC, grants from Humana, personal fees from Navvis Healthcare, personal fees from Elsevier Press, personal fees from Medicare Payment Advisory Commission, personal fees from Analysis Group, personal fees from Advocate Physician Partners, personal fees from the Federal Trade Commission, personal fees from Catholic Health Services Long Island, and equity from Clarify Health, personal fees and board membership for The Scan Group, and non-compensated board membership for Integrated Services, Inc. outside the submitted work in the past 3 years. Dr. Liao reports honoraria from Marcus Evans, Comagine Health, and Brown University outside the submitted work. Dr. Neville reports payments from the Commonwealth Fund and the Independent Health and Aged Care Pricing Authority of Australia and consulting fees from Capadev LLP. All other authors declare no conflicts of interest.
Disclaimer
This article does not necessarily represent the views of the US government or the Department of Veterans Affairs.
Prior presentations
-
1.
Society of General Internal Medicine Annual Meeting. Aurora, CO. May 11, 2023.
-
2.
AcademyHealth Annual Research Meeting. Seattle, WA. June 26, 2023.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crowley, A.P., Neville, S., Sun, C. et al. Differential Hospital Participation in Bundled Payments in Communities with Higher Shares of Marginalized Populations. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-024-08655-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-024-08655-4