Abstract
Objective
Determine whether patient-level or provider-level factors have greater influence on patient satisfaction scores in an academic general internal medicine clinic.
Methods
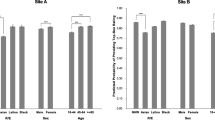
Two years of data (2017–2019) from the Clinician and Group Consumer Assessment of Healthcare Providers and Systems (CGCAHPS) surveys from ambulatory internal medicine clinic visits in an academic health center located in the Midwest United States were used. Patient satisfaction was measured using the overall provider satisfaction score (0–10), dichotomized with 9–10 defined as satisfactory and 0–8 as unsatisfactory. Provider-level independent variables included age, sex, race/ethnicity, provider type, service type, clinical effort, academic rank, and years since graduation. Patient-level factors included age, sex, race/ethnicity, education, and Epic Risk Score. Generalized mixed-effects logistic regression models were used to investigate associations between top-box satisfaction score and patient- and provider-level factors, accounting for the nesting of patients within providers.
Results
Thirty-three providers and 4597 patients were included in the analysis. Male providers (OR, 1.57; 95% CI, 1.00, 2.47), minority group 2 (OR, 3.54; 95% CI, 1.24, 10.07) and minority group 3 (OR, 6.04; 95% CI, 1.45, 25.12), faculty (OR, 3.83; 95% CI, 1.56, 9.36), and primary care providers (OR, 5.60; 95% CI, 1.62, 19.34) had increased odds of having a top-box rating compared with females, minority group 1, advanced practice providers, and perioperative providers respectively. Age was the only patient independent correlate of top-box rating with a 3% increased odds of top-box rating for every year increase in age (OR, 1.03; 95% CI 1.02, 1.03).
Conclusions
In this academic general internal medicine clinic, top-box satisfaction scores were more strongly associated with provider-level factors, including provider race/ethnicity, provider type, and service type, as opposed to patient-level factors. Further research is needed to confirm these findings and identify potential system-level interventions.

Similar content being viewed by others
Data Availability
A limited dataset that meets privacy and confidentiality standards of the institutional data is available from the corresponding author upon request.
References
Fenton JJ, Jerant A, Kravitz RL, et al. Reliability of Physician-Level Measures of Patient Experience in Primary Care. J Gen Intern Med. 2017;32(12):1323-1329.
Centers for Medicare and Medicaid Services. The hospital value-based purchasing program. Centers for Medicare and Medicaid Services: Baltimore, MD. 2021. Accessed from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HVBP/Hospital-Value-Based-Purchasing. Accessed January 29, 2024.
Holt JM. Patient Experience in Primary Care: A Systematic Review of CG-CAHPS Surveys. J Patient Exp. 2019;6(2):93-102.
Rave N, Geyer M, Reeder B, Ernst J, Goldberg L, Barnard C. Radical systems change. Innovative strategies to improve patient satisfaction. J Ambul Care Manage. 2003;26(2):159–174.
Nelson C, Niederberger J. Patient satisfaction surveys: an opportunity for total quality improvement. J Healthcare Manag. 1990;35(3):409-427.
Mehta SJ. Patient satisfaction reporting and its implications for patient care. AMA J Ethics 2015;17(7):616-621
Yaraghi N, Wang W, Gao G, Agarwal R. How online quality ratings influence patients' choice of medical providers: controlled experimental survey study. J Med Internet Res. 2018;20(3):e99.
Browne K, Roseman D, Shaller D, Edgman-Levitan S. Analysis & commentary. Measuring patient experience as a strategy for improving primary care. Health Aff (Millwood). 2010;29(5):921–5. https://doi.org/10.1377/hlthaff.2010.0238. PMID: 20439881.
Mukherjee S, Rodriguez HP, Elliott MN, Crane PK. Modern psychometric methods for estimating physician performance on the Clinician and Group CAHPS® survey. Health Serv Outcomes Res Methodol. 2013;13(2):109-23.
Agency for Healthcare Research and Quality. CAHPS Clinician and Group Survey- Version: Adult Visit Survey 4.0(Beta). Agency for Healthcare and Quality: Rockville, MD. 2020. Accessed from: https://www.ahrq.gov/sites/default/files/wysiwyg/cahps/surveys-guidance/cg/adult-eng-cg40-3351a.pdf. Accessed on: January 5, 2024.
Batbaatar E, Dorjdagva J, Luvsannyam A, Savino MM, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137(2):89-101.
Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur. 2009;22(4):366-81. https://doi.org/10.1108/09526860910964834.
Jaipaul CK, Rosenthal GE. Are older patients more satisfied with hospital care than younger patients? J General Internal Med. 2003;18(1):23-30.
Liljas AEM, Brattstrom F, Burstrom B, Schon P, Agerholm J. Impact of integrated care on patient-related outcomes among older people – a systematic review. Int J Integr Care. 2019;19(3):6.
Mazurenko O, Collum T, Ferdinand A, Menachemi N. Predictors of Hospital Patient Satisfaction as Measured by HCAHPS: A Systematic Review. J Healthc Manag. 2017;62(4):272-283.
Gray M, Jones KG, Wright BJ. Patients With Health-Related Social Needs More Likely to Report Poor Clinic Experiences. J Patient Exp. 2021;8:23743735211008307.
Centers for Medicare and Medicaid Services. Hospital Consumer Assessment of Healthcare Providers and Systems: HCAHPS Tables and HCAHPS On-Line. Health Services Advisory Group: Baltimore, MD. 2023. Accessed from: https://www.cms.gov/data-research/research/consumer-assessment-healthcare-providers-systems/hospital-cahps-hcahps. Accessed on: January 5, 2024.
Agency for Healthcare Research and Quality. How to report results of the CAHPS clinician and group survey. Robert Wood Johnson Foundation: Rockville, MD. 2023. Accessed from: https://www.ahrq.gov/sites/default/files/wysiwyg/cahps/surveys-guidance/cg/cgkit/HowtoReportResultsofCGCAHPS080610FINAL.pdf. Accessed on January 5, 2024.
Donabedian A. The quality of care. How can it be assessed? JAMA 1988;260(12):1743-1748.
Hippisley-Cox J, Coupland C. Predicting risk of emergency admission to hospital using primary care data: derivation and validation of QAdmissions score. BMJ Open 2013;3(8):e003482. https://doi.org/10.1136/bmjopen-2013-003482.
Billings J. Choosing a model to predict hospital admission: an observational study of new variants of predictive models for case finding. BMJ Open. 2012a;3(8):e003352. https://doi.org/10.1136/bmjopen-2013-003352
Billings J. Development of a predictive model to identify inpatients at risk of re-admission within 30 days of discharge (PARR-30). BMJ Open 2012b;2(4):e001667. https://doi.org/10.1136/bmjopen-2012-001667
Otte SV. Improved Patient Experience and Outcomes: Is Patient-Provider Concordance the Key? J Patient Exp. 2022 May 29;9:23743735221103033. https://doi.org/10.1177/23743735221103033.
Davidson KW, Shaffer JA, Ye S, Falzon L, Emeruwa IO, Sundquist K, Inneh IA, Mascitelli SL, Manzano WM, Vawdrey DK, Ting HH. Interventions to improve hospital patient satisfaction with healthcare providers and systems: a systematic review. BMJ Qual Saf. 2017;26(7) 596-606.
Hurwitz HM, Mercer M, Rose SL. Interventions that improve patient experience evidenced by raising HCAHPS and CG-CAHPS scores: a narrative literature review. Pat Exp J. 2023;10(1):107-114.
Sergesketter AR, Shammas RL, Langdell HC, Yi VN, Geng Y, Patel A, Erdmann D. The Influence of Patient and Surgeon Characteristics on Press Ganey Provider Ratings in Plastic Surgery. Aesthet Surg J. 2023 Oct 12:sjad325
Khan HA, Rabah NM, Winkelman RD, Levin JM, Mroz TE, Steinmetz MP. The Impact of Preoperative Depression on Patient Satisfaction With Spine Surgeons in the Outpatient Setting. Spine (Phila Pa 1976). 2021;46(3):184–190.
Bleustein C, Rothschild DB, Valen A, Valatis E, Schweitzer L, Jones R. Wait times, patient satisfaction scores, and the perception of care. Am J Manag Care 2014;20(5):393-400.
Patterson BM, Eskildsen SM, Clement RC, et al. Patient Satisfaction Is Associated With Time With Provider But Not Clinic Wait Time Among Orthopedic Patients. Orthopedics 2017;40(1):43-48
Boylan MR, Riesgo AM, Paulino CB, Tejwani NC. Is Patient Satisfaction Associated with Objective Measures of Geriatric Hip Fracture Care? Bull Hosp Jt Dis. 2018;76(4):252-58.
Funding
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK118038, R01DK120861, Principal Investigator (PI): Leonard Egede, MD; K23DK132505, PI: Hawks; R21DK135965-01; PI: Dawson), National Institute on Minority Health and Health Disparities (R01MD013826, PI: Egede/Walker), and American Diabetes Association (11–22-JDFHD-01, PI: Dawson). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
LEE obtained funding for the study. LEE and RJW obtained, analyzed, and interpreted the data. LEE, RJW, AZD, and LH designed the study, drafted the article, and critically revised the manuscript for intellectual content. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dawson, A.Z., Hawks, L., Walker, R.J. et al. Differential Effect of Patient- and Provider-Level Factors on Patient Satisfaction Scores in Academic General Internal Medicine Clinics. J GEN INTERN MED (2024). https://doi.org/10.1007/s11606-024-08648-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-024-08648-3