Abstract
Background
No clinical tools currently exist to stratify patients’ risks of patient-directed discharge (PDD).
Objective
This study aims to identify trends and factors associated with PDD, representation, and readmission.
Design
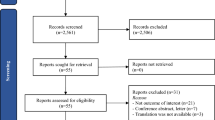
This was an IRB-approved, single-centered, retrospective study.
Participants
Patients aged > 18, admitted to medicine service, were included from January 1st through December 31st, 2019. Patients admitted to ICU or surgical services were excluded.
Main Measures
Demographics, insurance information, medical history, social history, rates of events occurrences, and discharge disposition were obtained.
Key Results
Of the 16,889 encounters, there were 776 (4.6%) PDDs, 4312 (25.5%) representations, and 2924 (17.3%) readmissions. Of those who completed PDDs, 42.1% represented and 26.4% were readmitted. Male sex, age ≤ 45, insurance type, homelessness, and substance use disorders had higher rates of PDD (OR = 2.0; 4.2; 4.5; 6.2; 5.2; p < 0.0001, respectively). Patients with homelessness, substance use disorders, mental health disorders, or prior history of PDD were more likely to represent (OR = 3.6; 2.0; 2.0; 1.5; p < 0.0001, respectively) and be readmitted (OR = 2.2; 1.6; 1.9; 1.5; p < 0.0001, respectively). Patients aged 30–35 had the highest PDD rate at 16%, but this was not associated with representations or readmissions. Between July and September, the PDD rate peaked at 5.5% and similarly representation and readmission rates followed. The rates of subsequent readmissions after PDDs were nearly two-fold compared to non-PDD patients in later half of the year. 51% of all subsequent readmissions occur within 7 days of PDD, compared to 34% in the non-PDD group (OR = 2.0; p < 0.0001). Patients with primary diagnosis of abscess had 16% PDDs.
Conclusions
Factors associated with PDD include male, younger age, insurance type, substance use, homelessness, and primary diagnosis of abscess. Factors associated with representation and readmission are homelessness, substance use disorders, mental health disorders, and prior history of PDD. Further research is needed to develop a risk stratification tool to identify at-risk patients.


Similar content being viewed by others
References
Spooner KK, Salemi JL, Salihu HM, Zoorob RJ. Discharge against medical advice in the United States, 2002-2011. Mayo Clin Proc. 2017;92(4):525-535.
Tan SY, Feng JY, Joyce C, Fisher J, Mostaghimi A. Association of hospital discharge against medical advice with readmission and in-hospital mortality. JAMA Netw Open. 2020;3(6):e206009.
Yong TY, Fok JS, Hakendorf P, Ben-Tovim D, Thompson CH, Li JY. Characteristics and outcomes of discharges against medical advice among hospitalised patients. Intern Med J. 2013;43(7):798-802.
Southern WN, Nahvi S, Arnsten JH. Increased Risk of Mortality and Readmission Among Patients Discharged Against Medical Advice. Am J Med. 2012;125(6):594-602. doi: https://doi.org/10.1016/j.amjmed.2011.12.017.
Garland A, Ramsey CD, Fransoo R, Olafson K, Chateau D, Yogendran M, Kraut A. Rates of readmission and death associated with leaving hospital against medical advice: a population-based study. CMAJ. 2013;185(14):1207-14.
Foster K, Caswell A, James L, Jessani H, Polanco A, Viggiano M, Jennings C, Yeung HM. The risk factors, consequences, and interventions of discharge against medical advice - a narrative review. Am J Med Sci. 2023;S0002-9629(23)01133-3.
Edwards J, Markert R, Bricker D. Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574-7.
Ibrahim SA, Kwoh CK, Krishnan E. Factors associated with patients who leave acute-care hospitals against medical advice. Am J Public Health. 2007;97(12):2204-8.
Baumrucker SJ, Carter GT, Stolick M, et al. Critically ill patient leaving against medical advice. Am J Hosp Palliat Care. 2018;35(11):1461-1466.
Temple University Hospital Community Benefit Report 2021-2022. Available at: https://issuu.com/templehealth/docs/tuhcommunitybenefitreport2021. Accessed April 2023.
American Hospital Association. June 2022 Metropolitan Anchor Hospital Case Study. Available at: https://www.aha.org/system/files/media/file/2022/10/Temple-University-Hospital-MAH-Case-Study.pdf. Accessed April 2023.
Lee CA, Cho JP, Choi SC, Kim HH, Park JO. Patients who leave the emergency department against medical advice. Clin Exp Emerg Med. 2016;3(2):88-94.
Akanbi O, Adejumo AC, Soliman M, Kudaravalli P. Chronic pancreatitis patients who leave against medical advice: prevalence, trend, and predictors. Dig Dis Sci. 2021;66(2):424-433.
Haywood C Jr, Lanzkron S, Ratanawongsa N, Bediako SM, Lattimer-Nelson L, Beach MC. Hospital self-discharge among adults with sickle-cell disease (SCD): associations with trust and interpersonal experiences with care. J Hosp Med. 2010 5(5):289-94.
Mishra AK, Abraham BM, Sahu KK, George AA, Sargent J, Kranis MJ, George SV, Abraham GM. Harms and contributors of leaving against medical advice in patients with infective endocarditis. J Patient Saf. 2022.
Villareal ME, Schubauer K, Paredes AZ, Santry HP, Tamer R, Strassels SA, Wisler J. Leaving against medical advice after emergency general surgery: avoiding a two-hit effect. J Surg Res. 2021;257:278-284.
Yuan S, Ashmore S, Chaudhary KR, Hsu B, Puumala SE. The role of socioeconomic status in individuals that leave against medical advice. S D Med. 2018;71(5):214-219.
Schaefer GR, Matus H, Schumann JH, Sauter K, Vekhter B, Meltzer DO, Arora VM. Financial responsibility of hospitalized patients who left against medical advice: medical urban legend? J Gen Intern Med. 2012;27(7):825-30.
Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: a qualitative study. Subst Abus. 2020;41(4):519-525.
Wung YT, Chen CC, Chen FC, Lin CH. Schizophrenia patients discharged against medical advice at a mental hospital in Taiwan. Psychiatry Clin Neurosci. 2010;64(4):415-20.
Samaras N, Chevalley T, Samaras D, Gold G. Older patients in the emergency department: a review. Ann Emerg Med. 2010;56(3):261-9.
Glans M, Kragh Ekstam A, Jakobsson U, Bondesson Å, Midlöv P. Risk factors for hospital readmission in older adults within 30 days of discharge - a comparative retrospective study. BMC Geriatr. 2020;20(1):467.
Berry JG, Gay JC, Joynt Maddox K, Coleman EA, Bucholz EM, O’Neill MR, Blaine K, Hall M. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ. 2018;360:k497.
Akintoye E, Briasoulis A, Egbe A, Adegbala O, Alliu S, Sheikh M, Singh M, Ahmed A, Mallikethi-Reddy S, Levine D. Seasonal variation in hospitalization outcomes in patients admitted for heart failure in the United States. Clin Cardiol. 2017;40(11):1105-1111.
Gautam N, Sharma JP, Sharma A, Verma V, Arora P, Gautam PL. Retrospective evaluation of patients who leave against medical advice in a tertiary teaching care institute. Indian J Crit Care Med. 2018;22(8):591-596.
Blecker S, Kwon JY, Herrin J, Grady JN, Horwitz LI. Seasonal variation in readmission risk for patients hospitalized with cardiopulmonary conditions. J Gen Intern Med. 2018;33(5):599-601.
Kimmel SD, Kim JH, Kalesan B, Samet JH, Walley AY, Larochelle MR. Against medical advice discharges in injection and non-injection drug use-associated infective endocarditis: a nationwide cohort study. Clin Infect Dis. 2021;73(9):e2484-e2492.
Nolan NS, Marks LR, Liang SY, Durkin MJ. Medications for opioid use disorder associated with less against medical advice discharge among persons who inject drugs hospitalized with an invasive infection. J Addict Med. 2021;15(2):155-158.
Prescott HC, Sjoding MW, Iwashyna TJ. Diagnoses of early and late readmissions after hospitalization for pneumonia. A systematic review. Ann Am Thorac Soc. 2014;11(7):1091-100.
Weiss AJ (IBM Watson Health), Jiang HJ (AHRQ). Overview of clinical conditions with frequent and costly hospital readmissions by payer, 2018. HCUP Statistical Brief #278. July 2021. Agency for Healthcare Research and Quality, Rockville, MD
Aydin H, Doğan H. COVID-19 outbreak impact on discharge against medical advice from the ED: a retrospective study. Am J Emerg Med. 2022;57:21-26.
Lemstra M, Mackenbach J, Neudorf C, Nannapaneni U. High health care utilization and costs associated with lower socio-economic status: results from a linked dataset. Can J Public Health. 2009;100(3):180-3.
Schickedanz A, Sharp A, Hu YR, Shah NR, Adams JL, Francis D, Rogers A. Impact of social needs navigation on utilization among high utilizers in a large integrated health system: a quasi-experimental study. J Gen Intern Med. 2019;34(11):2382-2389.
Saeed S, Patel R, Odeyemi R. Calibrating readmission risk prediction models for determining post-discharge follow-up timing. J Community Hosp Intern Med Perspect. 2022;12(4):24-27.
Acknowledgements:
We thank Drs. Yazan Bittar and Aidan Pearigen for their efforts in data collection and verification.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yeung, HM., Ifrah, A. & Rockman, M.E. Quantitative Analysis of Characteristics Associated with Patient-Directed Discharges, Representations, and Readmissions: a Safety-Net Hospital Experience. J GEN INTERN MED 39, 1173–1179 (2024). https://doi.org/10.1007/s11606-023-08563-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08563-z