Abstract
Background
The FDA issued a “black box” warning regarding risks of fluoroquinolones in 2008 with updates in 2011, 2013, and 2016.
Objective
To examine antimicrobial use in hospital-treated UTIs from 2000 to 2020.
Design
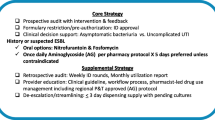
Cross-sectional study with interrupted time series analysis.
Participants
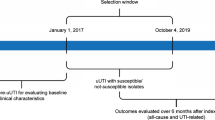
Patient encounters with a diagnosis of UTI from January 2000 to March 2020, excluding diagnoses of renal abscess, chronic cystitis, and infection of the gastrointestinal tract, lungs, or prostate.
Main Measures
Monthly use of fluoroquinolone and non-fluoroquinolone antibiotics were assessed. Fluoroquinolone resistance was assessed in available cultures. Interrupted time series analysis examined level and trend changes of antimicrobial use with each FDA label change.
Key Results
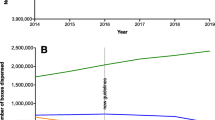
A total of 9,950,790 patient encounters were included. From July 2008 to March 2020, fluoroquinolone use declined from 61.7% to 11.7%, with similar negative trends observed in inpatients and outpatients, age ≥ 60 and < 60 years, males and females, patients with and without pyelonephritis, and across physician specialties. Ceftriaxone use increased from 26.4% encounters in July 2008 to 63.6% of encounters in March 2020. Among encounters with available culture data, fluoroquinolone resistance declined by 28.9% from 2009 to 2020. On interrupted time series analysis, the July 2008 FDA warning was associated with a trend change (-0.32%, < 0.001) and level change (-5.02%, p < 0.001) in monthly fluoroquinolone use.
Conclusions
During this era of “black box” warnings, there was a decline in fluoroquinolone use for hospital-treated UTI with a concomitant decline in fluoroquinolone resistance and rise in ceftriaxone use. Efforts to restrict use of a medication class may lead to compensatory increases in use of a single alternative agent with changes in antimicrobial resistance profiles.




Similar content being viewed by others
Data Availability
The data that support the findings of this study are from the Premier Healthcare Database, a commercially available database that cannot be made public, but is available for purchase.
References
Tanne JH. FDA adds "black box" warning label to fluoroquinolone antibiotics. BMJ. 2008;337(7662):a816. Published 2008 Jul 15. https://doi.org/10.1136/bmj.a816.
FDA Updates Warnings for Fluoroquinolone Antibiotics. U.S. Food and Drug Administration, FDA, https://www.fda.gov/news-events/press-announcements/fda-updates-warnings-fluoroquinolone-antibiotics. Accessed 29 Dec 2021.
Tran PT, Antonelli PJ, Hincapie-Castillo JM, Winterstein AG. Association of US Food and Drug Administration removal of indications for use of oral quinolones with prescribing trends. JAMA Intern Med. 2021;181(6):808-816. https://doi.org/10.1001/jamainternmed.2021.1154.
Sankar A, Swanson KM, Zhou J, et al. Association of fluoroquinolone prescribing rates with black box warnings from the US Food and Drug Administration. JAMA Netw Open. 2021;4(12):e2136662. https://doi.org/10.1001/jamanetworkopen.2021.36662.
Jeong IG, Khandwala YS, Kim JH, et al. Association of robotic-assisted vs laparoscopic radical nephrectomy with perioperative outcomes and health care costs, 2003 to 2015. JAMA. 2017;318(16):1561-1568.
Xiong S, Liu X, Deng W, Zhou Z, Li Y, Tu Y, Chen L, Wang G, Fu B. Pharmacological interventions for bacterial prostatitis. Front Pharmacol. 2020;11:504. https://doi.org/10.3389/fphar.2020.00504.
Widen A, Waldman B. Petition for a Black Box Warning on Fluoroquinolone Antibiotics. Public Citizen, 29 Aug. 2006, https://www.citizen.org/article/petition-for-a-black-box-warning-on-fluoroquinolone-antibiotics/. Accessed 3 Feb 2022.
McFarland LV, Clarridge JE, Beneda HW, Raugi GJ. Fluoroquinolone use and risk factors for Clostridium difficile-associated disease within a Veterans Administration health care system. Clin Infect Dis. 2007;45(9):1141-1151. https://doi.org/10.1086/522187.
Pépin J, Saheb N, Coulombe MA, et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis. 2005;41(9):1254-1260. https://doi.org/10.1086/496986.
Park SH. Third-generation cephalosporin resistance in gram-negative bacteria in the community: a growing public health concern. Korean J Intern Med. 2014;29(1):27-30. https://doi.org/10.3904/kjim.2014.29.1.27.
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629-655. https://doi.org/10.1016/S0140-6736(21)02724-0.
Rubino A, Sanon M, Ganz ML, et al. Association of the US Food and Drug Administration antipsychotic drug boxed warning with medication use and health outcomes in elderly patients with dementia. JAMA Netw Open. 2020;3(4):e203630. Published 2020 Apr 1. https://doi.org/10.1001/jamanetworkopen.2020.3630.
Yarrington ME, Anderson DJ, Dodds Ashley E, et al. Impact of FDA black box warning on fluoroquinolone and alternative antibiotic use in southeastern US hospitals. Infect Control Hosp Epidemiol. 2019;40(11):1297-1300. https://doi.org/10.1017/ice.2019.247.
Ebell MH. Treating adult women with suspected UTI. Am Fam Physician. 2006;73(2):293-296.
Lee RA, Centor RM, Humphrey LL, et al. Appropriate use of short-course antibiotics in common infections: best practice advice from the American College of Physicians. Ann Intern Med. 2021;174(6):822-827. https://doi.org/10.7326/M20-7355.
Anger J, Lee U, Ackerman AL, et al. Recurrent uncomplicated urinary tract infections in women: AUA/CUA/SUFU Guideline. J Urol. 2019;202(2):282-289. https://doi.org/10.1097/JU.0000000000000296.
Acknowledgements:
Jonathan Shoag is supported by the Frederick J. and Theresa Dow Fund of the New York Community Trust, the Vinney Scholars Award, and a Damon Runyon Cancer Research Foundation Physician Scientist Training Award. The work presented here was not directly funded by an outside organization or sponsor. Jonathan Shoag had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors of this manuscript have no financial interests or relationships relevant to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors of this transcript have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brant, A., Lewicki, P., Wu, X. et al. Antibiotic Use in Hospital Urinary Tract Infections After FDA Regulation. J GEN INTERN MED (2023). https://doi.org/10.1007/s11606-023-08559-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11606-023-08559-9