Abstract
Introduction
Methadone ameliorates opioid withdrawal among hospitalized patients with opioid use disorder (OUD). To continue methadone after hospital discharge, patients must enroll in an opioid treatment program (OTP) per federal regulations. Uncontrolled opioid withdrawal is a barrier to linkage from hospital to OTP.
Aim
Describe a federally compliant In-Hospital Methadone Enrollment Team (IN-MEET) that enrolls hospitalized patients with OUD into an OTP with facilitated hospital to OTP linkage.
Setting
Seven hundred-bed university hospital in Aurora, CO.
Program Description
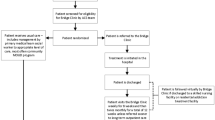
A physician dually affiliated with a hospital’s addiction consultation service and a community OTP completes an in-hospital, face-to-face medical assessment required by federal law and titrates methadone to comfort. An OTP-affiliated nurse with hospital privileges completes a psychosocial evaluation and provides case management by arranging transportation and providing weekly telephone check-ins.
Program Evaluation Metrics
IN-MEET enrollments completed, hospital to OTP linkage, and descriptive characteristics of patients who completed IN-MEET enrollments compared to patients who completed community OTP enrollments.
Results
Between April 2019 and April 2023, our team completed 165 IN-MEET enrollments. Among a subset of 73 IN-MEET patients, 56 (76.7%) presented to the OTP following hospital discharge. Compared to community OTP enrolled patients (n = 1687), a higher percentage of IN-MEET patients were older (39.7 years, standard deviation [SD] 11.2 years vs. 36.1 years, SD 10.6 years) and were unhoused (n = 43, 58.9% vs. n = 199, 11.8%). Compared to community OTP enrolled patients, a higher percentage of IN-MEET patients reported heroin or fentanyl as their primary substance (n = 53, 72.6% vs. n = 677, 40.1%), reported methamphetamine as their secondary substance (n = 27, 37.0% vs. n = 380, 22.5%), and reported they injected their primary substance (n = 46, 63.0% vs. n = 478, 28.3%).
Conclusion
IN-MEET facilitates hospital to OTP linkage among a vulnerable population. This model has the potential to improve methadone access for hospitalized patients who may not otherwise seek out treatment.

Similar content being viewed by others
Data Availability
Data are available upon request.
References
Ahmad FB CJ, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. 2023. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed 21 Aug 2023.
Singh JA, Cleveland JD. National U.S. time-trends in opioid use disorder hospitalizations and associated healthcare utilization and mortality. PLoS ONE. 2020;15(2):e0229174. https://doi.org/10.1371/journal.pone.0229174.
Calcaterra SL, Martin M, Bottner R, et al. Management of opioid use disorder and associated conditions among hospitalized adults: A Consensus Statement from the Society of Hospital Medicine. J Hosp Med. 2022;17(9):744-756. https://doi.org/10.1002/jhm.12893.
Calcaterra SL, Bottner R, Martin M, et al. Management of opioid use disorder, opioid withdrawal, and opioid overdose prevention in hospitalized adults: A systematic review of existing guidelines. J Hosp Med. 2022;17(9):679-692.
Alrawashdeh M, Rhee C, Klompas M, et al. Association of early opioid withdrawal treatment strategy and patient-directed discharge among hospitalized patients with opioid use disorder. J Gen Intern Med. 2023. https://doi.org/10.1007/s11606-023-08059-w.
Bredenberg E, Tietbohl C, Dafoe A, Thurman L, Calcaterra S. Identifying factors that contribute to burnout and resilience among hospital-based addiction medicine providers: A qualitative study. J Subst Abuse Treat. 2023;144:108924. https://doi.org/10.1016/j.jsat.2022.108924.
Calcaterra SL, Lockhart S, Callister C, Hoover K, Binswanger IA. Opioid use disorder treatment initiation and continuation: a qualitative study of patients who received addiction consultation and hospital-based providers. J Gen Intern Med. 2022. https://doi.org/10.1007/s11606-021-07305-3.
Englander H, Dobbertin K, Lind BK, et al. Inpatient addiction medicine consultation and post-hospital substance use disorder treatment engagement: a propensity-matched analysis. J Gen Intern Med. 2019;34(12):2796–2803. https://doi.org/10.1007/s11606-019-05251-9.
Trowbridge P, Weinstein ZM, Kerensky T, et al. Addiction consultation services - Linking hospitalized patients to outpatient addiction treatment. J Subst Abuse Treat. 2017;79:1-5. https://doi.org/10.1016/j.jsat.2017.05.007.
Wakeman SE, Larochelle MR, Ameli O, et al. Comparative effectiveness of different treatment pathways for opioid use disorder. JAMA Netw Open. 2020;3(2):e1920622-e1920622. https://doi.org/10.1001/jamanetworkopen.2019.20622.
Tierney HR, Rowe CL, Coffa DA, Sarnaik S, Coffin PO, Snyder HR. Inpatient opioid use disorder treatment by generalists is associated with linkage to opioid treatment programs after discharge. J Addict Med. 2022;16(2):169-176.
Christian N, Bottner R, Baysinger A, et al. Hospital buprenorphine program for opioid use disorder is associated with increased inpatient and outpatient addiction treatment. J Hosp Med. 2021;16(6):345-348.
D’Onofrio G, O’Connor PG, Pantalon MV, et al. Emergency department-initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. Jama. 2015;313(16):1636-44. https://doi.org/10.1001/jama.2015.3474.
Englander H, Priest KC, Snyder H, Martin M, Calcaterra S, Gregg J. A call to action: hospitalists’ role in addressing substance use disorder. J Hosp Med. 2020;15(3):184-187. https://doi.org/10.12788/jhm.3311.
U.S. Department of Justice DEA, Diversion Control Division. Title 21 Code of Federal Regulations 1306.07: Administering or dispensing of narcotic drugs. United States Drug Enforcement Administration. July 29, 2022. Updated 2020. https://www.govinfo.gov/content/pkg/CFR-1998-title21-vol9/xml/CFR-1998-title21-vol9-sec1306-07.xml. Accessed 8 Aug 2023.
Martin M, Englander H, Calcaterra SL. Things We Do for No Reason™: Avoiding methadone for opioid withdrawal. J Hosp Med. 2023. https://doi.org/10.1002/jhm.13138.
Substance Abuse and Mental Health Services Administration. Federal Guidelines for Opioid Treatment Programs. HHS Publication No. (SMA) XX-XXXX. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2015.
Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169(3):137-145. https://doi.org/10.7326/m17-3107.
Hoover K, Lockhart S, Callister C, Holtrop JS, Calcaterra SL. Experiences of stigma in hospitals with addiction consultation services: A qualitative analysis of patients’ and hospital-based providers’ perspectives. J Subst Abuse Treat. 2022;138:108708. https://doi.org/10.1016/j.jsat.2021.108708.
Calcaterra S, Bach P, Chadi A, et al. Methadone matters: what the United States can learn from the global effort to treat opioid addiction. J Gen Intern Med. 2019;34(6):1039-1042.
Joudrey PJ, Chadi N, Roy P, et al. Pharmacy-based methadone dispensing and drive time to methadone treatment in five states within the United States: A cross-sectional study. Drug Alcohol Depend. 2020;211:107968. https://doi.org/10.1016/j.drugalcdep.2020.107968.
Joudrey PJ, Edelman EJ, Wang EA. Drive times to opioid treatment programs in urban and rural counties in 5 US States. JAMA. 2019;322(13):1310-1312. https://doi.org/10.1001/jama.2019.12562.
Davis CS, Carr DH. Legal and policy changes urgently needed to increase access to opioid agonist therapy in the United States. Int J Drug Policy. 2019;73:42-48. https://doi.org/10.1016/j.drugpo.2019.07.006.
Tierney HR, Takimoto SW, Azari S, Steiger S, Martin M. Predictors of Linkage to an opioid treatment program and methadone treatment retention following hospital discharge in a safety-net setting. Subst Use Misuse. 2023;58(9):1172-1176. https://doi.org/10.1080/10826084.2023.2212070.
Calcaterra SL, McBeth L, Keniston AM, Burden M. The development and implementation of a hospitalist-directed addiction medicine consultation service to address a treatment gap. J Gen Intern Med. 2022;37(5):1065-1072. https://doi.org/10.1007/s11606-021-06849-8.
University of Colorado SoM, Department of Psychiatry. Addiction Research and Treatment Services (ARTS). 2022. https://www.artstreatment.com/. Accessed 8 Aug 2023.
Davis CS, Carr DH. Legal and policy changes urgently needed to increase access to opioid agonist therapy in the United States. Int J Drug Policy. 2019/11/01/ 2019;73:42–48. https://doi.org/10.1016/j.drugpo.2019.07.006.
Request for Exception to Limitations on Dispensing for OUD (2023). https://www.deadiversion.usdoj.gov/drugreg/Instructions-to-request-exception-to-21-CFR%201306.07(b)-3-day-rule-(EO-DEA248R1).pdf.
Steadman PYD. SB16-202: Increasing Access Effective Substance Use Services. In: 73rd General Assembly CGA, editor. SB16-202. Denver, Colorado, 2016. p. 5. https://leg.colorado.gov/bills/sb16-202.
Dennis M. The Global Appraisal of Individual Needs (GAIN) Progressive Approach to Assessment. https://gaincc.org/about/. Accessed 31 May 2023.
DACODS User Manual (Drug and Alcohol Coordinated Data System) (2022). https://adad.cdhs.state.co.us/Training/DACODS%20User%20Manual,%20revised%2012222009.pdf.
Liebschutz JM, Crooks D, Herman D, et al. Buprenorphine treatment for hospitalized, opioid-dependent patients: a randomized clinical trial. JAMA Intern Med. 2014;174(8):1369-76. https://doi.org/10.1001/jamainternmed.2014.2556.
Christian N, Bottner R, Baysinger A, et al. Hospital buprenorphine program for opioid use disorder is associated with increased inpatient and outpatient addiction treatment. J Hosp Med. 2021;16(6):345-348. https://doi.org/10.12788/jhm.3591.
Wadhera RK, Choi E, Shen C, Yeh RW, Joynt Maddox KE. Trends, causes, and outcomes of hospitalizations for homeless individuals: a retrospective cohort study. Med Care. 2019;57(1):21-27. https://doi.org/10.1097/mlr.0000000000001015.
Glick SN, Klein KS, Tinsley J, Golden MR. Increasing heroin-methamphetamine (goofball) use and related morbidity among seattle area people who inject drugs. Am J Addict. 2021;30(2):183-191. https://doi.org/10.1111/ajad.13115.
Korthuis PT, Cook RR, Foot CA, et al. Association of methamphetamine and opioid use with nonfatal overdose in rural communities. JAMA Network Open. 2022;5(8):e2226544-e2226544. https://doi.org/10.1001/jamanetworkopen.2022.26544.
Han B, Compton WM, Jones CM, Einstein EB, Volkow ND. Methamphetamine use, methamphetamine use disorder, and associated overdose deaths among US adults. JAMA Psychiatry. 2021;78(12):1329-1342. https://doi.org/10.1001/jamapsychiatry.2021.2588.
Silverstein SM, Daniulaityte R, Getz K, Zule W. “It’s crazy what meth can help you do”: lay beliefs, practices, and experiences of using methamphetamine to self-treat symptoms of opioid withdrawal. Subst Use Misuse. 2021;56(11):1687-1696. https://doi.org/10.1080/10826084.2021.1949612.
Bungay V, Malchy L, Buxton JA, Johnson J, MacPherson D, Rosenfeld T. Life with jib: A snapshot of street youth’s use of crystal methamphetamine. Addict Res Theory. 2006;14(3):235–251. https://doi.org/10.1080/16066350500270901.
Ivsins A, Fleming T, Barker A, et al. The practice and embodiment of “goofballs”: A qualitative study exploring the co-injection of methamphetamines and opioids. Int J Drug Policy. 2022;107:103791. https://doi.org/10.1016/j.drugpo.2022.103791.
Funding
Dr. Calcaterra is supported by the National Institute on Drug Abuse (NIDA), National Institutions of Health, grant award number K08DA049905. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health. IN-MEET is funded by Colorado State Bill 16-202, “Increasing Access Effective Substance Use Services”.
National Institute on Drug Abuse,K08DA049905,Susan Calcaterra
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Calcaterra, S.L., Saunders, S., Grimm, E. et al. In-Hospital Methadone Enrollment: a Novel Program to Facilitate Linkage from the Hospital to the Opioid Treatment Program for Vulnerable Patients with Opioid Use Disorder. J GEN INTERN MED 39, 385–392 (2024). https://doi.org/10.1007/s11606-023-08411-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08411-0