Abstract
Background
High-need, high-cost Medicare patients can have difficulties accessing office-based primary care. Home-based primary care (HBPC) can reduce access barriers and allow a clinician to obtain valuable information not obtained during office visit, possibly leading to reductions in hospital use.
Objective
To determine whether HBPC for high-need, high-cost patients reduces hospitalizations and Medicare inpatient expenditures.
Design
We conducted a matched retrospective cohort study using a difference-in-differences analysis to examine patients 2 years before and 2 years after their first home visit (HBPC group).
Participants
The study included high-need, high-cost fee-for-service Medicare patients without prior HBPC use, of which 55,303 were new HBPC recipients and 156,142 were matched comparison patients.
Intervention
Receipt of at least two HBPC visits and, within 6 months of the index HBPC visit, a majority of a patient’s primary care visits in the home.
Main Measures
Total and potentially avoidable hospitalizations and Medicare inpatient expenditures.
Key Results
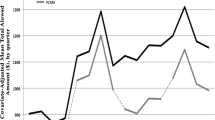
HBPC reduced total hospitalization rates, but the marginal effects were not statistically significant: a reduction of 11 total hospitalizations per 1000 patients in the first year (− 0.6%, p = 0.19) and 14 in the second year (− 0.7%, p = 0.16). However, HBPC reduced potentially avoidable hospitalization rates in the second year. The estimated marginal effect was a reduction of 6 potentially avoidable hospitalizations per 1000 patients in the first year (− 1.6%, p = 0.16) and 11 in the second (− 3.1%, p = 0.01). The estimated effect of HBPC was a small decrease in inpatient expenditures of $24 per patient per month (− 1.1%, p = 0.10) in the first year and $0 (0.0%, p = 0.99) in the second.
Conclusions
After high-need, high-cost patients started receiving HBPC, they did not experience fewer total hospitalizations or lower inpatient spending but may have had lower rates of potentially avoidable hospitalizations after 2 years.


Similar content being viewed by others
Data Availability
The data sets used to create the analysis file for the current study are available through a data use agreement with the Centers for Medicare & Medicaid Services.
References
Hayes SL, Salzberg CA, McCarthy D, et al. High-need, high-cost patients: who are they and how do they use health care? 2016. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2016/aug/high-need-high-cost-patients-who-are-they-and-how-do-they-use. Accessed 9 June 2023.
Joynt KE, Gawande AA, Orav J, Jha AK. Contribution of preventable acute care spending to total spending for high-cost medicare patients. JAMA. 2013;309:2572–78.
Zimbroff RM, Ornstein KA, Sheehan OC. 2021. Home-based primary care: a systematic review of the literature, 2010-2020. J Am Geriatr Soc. 2021;69:2963–72.
Leff B, Weston CM, Garrigues S, et al. Home-based primary care practices in the United States: current state and quality improvement approaches. J Am Geriatr Soc. 2015;63:963–69.
Hulen M, Laliberte A, Ono S, Saha S, Edwards ST. “Eyes in the home”: addressing social complexity in Veterans Affairs home-based primary care. J Gen Int Med. 2021;36:894–900.
Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:161–240.
Covinsky KE, Palmer, RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–58.
Reckrey, JM, Yang M, Kinosian B, et al. Receipt of home-based medical care among older beneficiaries enrolled in Fee-for-Service Medicare. Health Aff. 2020;39:1289-96.
Kimmey, L, Anderson, M, Cheh V, et al. “Evaluation of the Independence at Home Demonstration: an examination of the first four years.” Washington, DC: Mathematica. 2019. Available at https://innovation.cms.gov/initiatives/independence-at-home/. Accessed 9 June 2023.
Federman, AD, Brody A, Ritchie CS, et al. Outcomes of home-based primary care for homebound older adults: a randomized clinical trial. J Am Geriatr Soc. 2023;71:334–454.
Yao N, Rose K, LeBaron V, Camacho F, Boling P. Increasing role of nurse practitioners in house call programs. J Am Geriatr Soc. 2017;65:847–2.
Klein S, Hostetter M, McCarthy D. An overview of home-based primary care: learning from the field. 2017. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2017/jun/overview-home-based-primary-care-learning-field. Accessed 5 October 2022.
Yao N, Mutter JB, Berry JD, Yamanaka T, Mohess DT, Cornwell T. In traditional Medicare, modest growth in the home care workforce largely driven by nurse practitioners. Health Aff. 2021:40;478–86.
Ornstein KA, Garrido MM, Bollens-Lund E, et al. Estimation of the incident homebound population in the US among older Medicare beneficiaries, 2012 to 2018. JAMA Intern Med. 2020;180:1022–25.
Liu B, Ritchie CS, Ankuda CK, et al. Growth of fee-for-service Medicare home-based medical care within private residences and domiciliary care settings in the U.S., 2012–2019. J Am Med Dir Assoc. 2020;23:1614–20.
Acknowledgements:
The authors acknowledge the significant contributions to a predecessor of this study that were provided by the following former Mathematica employees: Valerie Cheh and Catherine McLaughlin.
Funding
This study was funded by the Centers for Medicare & Medicaid Services under contract number HHSM-500–2014-00034I/HHSM-500-T0018. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Health and Human Services or any of its agencies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest:
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information:
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kimmey, L., Wysocki, A., Forrow, L.V. et al. Effects of Home-Based Primary Care on Hospital Use for High-Need Medicare Patients: an Observational Study. J GEN INTERN MED 39, 19–26 (2024). https://doi.org/10.1007/s11606-023-08328-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08328-8